Home Visits: Free Templates - SafetyCulture
32 hours ago · If you’re efficient, you can often complete the entire note during the home health visit! Reassessment Note – In Home Health therapy, reassessments are basically like a progress note and take a little longer than a regular visit to complete. Plan to spend 45 to 60 minutes with the patient and up to 20-30 minutes to complete a reassessment note. >> Go To The Portal
When to fill out visit notes for a home health aide?
Most home health aides are required to document their care on visit notes. If you care for clients in their homes, be sure to complete your visit notes at the time of each home visit. Don’t wait until the end of the day to fill out visit notes on all your clients.
How do you write the time for a home health visit?
Note the time of your arrival and your departure from each client’s home (if you make home health visits). Use the proper time format according to your workplace policy. For example, some health care organizations use a twelve hour clock, noting whether it’s AM or PM. Others use a twenty-four hour clock—also called military time.
What is the objective of home visits in healthcare?
The objective of home visits is to provide medical service at your doorsteps. According to 2013 home visits health care benchmark, the following are the top components of home visits: Medication Reconciliation – is a process of accurate listing of patient’s medication that has been compared to medical orders or patient’s records.
What do you need to know about home health documentation?
Special Tips For Home Health Documentation: Home health clients on Medicare must be homebound—and must need help with bathing—to receive the services of a home health aide. Your documentation should show that your client meets these requirements.
How do you write a visit frequency for home health?
0:0011:35How to Write a Home Health Frequency - YouTubeYouTubeStart of suggested clipEnd of suggested clipDr. Smith physical therapist here and today I'm going to teach you how to properly write a homeMoreDr. Smith physical therapist here and today I'm going to teach you how to properly write a home health frequency for patients on Medicare Part A services.
How do I write a night shift report?
5 Tips for an Effective End-of-Shift ReportGive a Bedside Report. “Check pertinent things together such as skin, neuro, pulses, etc. ... Be Specific, Concise and Clear. “Stay on point with the 'need to know' information. ... When in Doubt, Ask for Clarification. ... Record Everything. ... Be Positive!
What should you remember when you are documenting?
Medical Documenting: 5 Important Things to RememberWrite Clearly and Legibly. According to a report in Medscape, the modern health care system puts increasing demands on nurses' time. ... Handle Records with Care. ... Document All Your Actions. ... Record Only Objective Facts. ... Capture Orders Correctly.
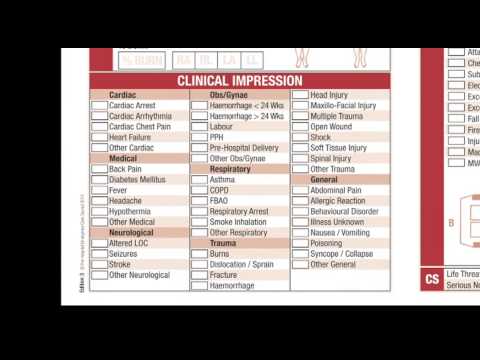
What are some common diagnosis in home care?
Common diagnoses among home health care patients include circulatory disease (31 percent of patients), heart disease (16 percent), injury and poisoning (15.9 percent), musculoskeletal and connective tissue disease (14.1 percent), and respiratory disease (11.6 percent).
How do you give a good report?
1:2020:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd what I do with my report should sheet. At the end of the day I always tread it so tip alwaysMoreAnd what I do with my report should sheet. At the end of the day I always tread it so tip always shred your report sheet whenever you're done giving a report you don't want to stick it in your locker.
What should a shift report include?
It should include the patient's medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
What are the 3 rules of documentation?
Documentation should be:Immediate. Managers should take notes right after an incident occurs. ... Accurate and believable. When an outside observer (judge, jury or EEO investigator) is called to judge your side of the story, detailed observations add authenticity. ... Agreed upon.
How do you document a patient chart?
Tips for Patient ChartingUse Evidence-Based Care Plans. ... Document Patient Care Using Standard Medical Terminology. ... Avoid Using Restricted Abbreviations in Patient Charting. ... Save Time by Integrating Technology. ... Use the HER's Dictation Functionality. ... Document to Medical Necessity.More items...•
What is the golden rule of chart documentation?
Remember the Golden Rule: If it isn't documented, then it wasn't performed. Reviewers do not know the services provided if there is no documentation. You are paid for what you document, not what you did.
Which is the primary goal of home health care?
The primary goal of home health care is to help the client function within limitations. Home health care allows people to regain or maintain optimal health and to remain in the home environment.
What does the primary diagnosis represent in home health?
The primary diagnosis is defined as the “chief reason the patient is receiving home care” and the diagnosis most related to the current home care POC.
What are patient centered goals?
The goal of patient-centered health care is to empower patients to become active participants in their care. This requires that physicians, radiologic technologists and other health care providers develop good communication skills and address patient needs effectively.
Home Health Documentation Examples
The amount of time it takes to write home health physical therapy documentation (and occupational therapy documentation) will vary depending on the type of note you’re writing.
Download the Home Health Documentation Templates
If you’re a new home health therapist, this guide will save you time and headache as you can actually spend more time focusing on the patient’s needs and treatment.
Therapy Documentation Template Bundle
I mentioned that I spent an entire year crafting my templates and creating a system that saved me time. You can see the entire system in the bundle below, which includes:
What is the purpose of documentation?
Remember, the purpose of documentation is to communicate with other members of the health care team. (If you are the only person who can read your handwriting, your documentation won’t communicate anything to anybody!)
How often should you document vitals?
Patients in acute care settings tend to be quite sick. If you are ordered to document vital signs every four hours, it’s important to take the vitals—and document the results—on time.
Do Medicare clients need to bathe?
Home health clients on Medicare must be homebound—and must need help with bathing— to receive the services of a home health aide. Your documentation should show that your client meets these requirements. However, if your client has already bathed when you arrive, document the reason and tell your supervisor right away.