Individuals’ Right under HIPAA to Access their Health …
28 hours ago With limited exceptions, the HIPAA Privacy Rule gives individuals the right to access, upon request, the medical and health information (protected health information or PHI) about them in one or more designated record sets maintained by or for the individuals’ health care providers and health plans (HIPAA covered entities). >> Go To The Portal
Full Answer
What are the HIPAA regulations for medical records?
HIPAA regulations for medical records dictate the mandatory data storage and release policies that all healthcare institutions have to comply with. As a federal law, HIPAA is governed by the Department of Health and Human Services (HHS). However, the HIPAA regulations for medical records retention and release may differ in different states.
What information can be included in a HIPAA form?
Understanding HIPAA for Dummies Names or part of names Any other unique identifying characteris ... Geographical identifiers Dates directly related to a person Phone number details Fax number details Details of Email addresses Social Security details Medical record numbers Health insurance beneficiary numbers 4 more rows ...
What are the HIPAA implications for patients?
The HIPAA implications for patients are that their healthcare information is treated more sensitively and can be accessed more quickly by their healthcare suppliers.
What is protected health information under HIPAA?
Protected Health Information. The Privacy Rule protects all "individually identifiable health information" held or transmitted by a covered entity or its business associate, in any form or media, whether electronic, paper, or oral. The Privacy Rule calls this information "protected health information (PHI)."
What is summary health information under HIPAA?
“Summary health information” is information that summarizes claims history, claims expenses, or types of claims experience of the individuals for whom the plan sponsor has provided health benefits through the group health plan, and that is stripped of all individual identifiers other than five digit zip code (though it ...
Is the patient record included in the protected health information?
In other words, PHI is personally identifiable information in medical records, including conversations between doctors and nurses about treatment. PHI also includes billing information and any patient-identifiable information in a health insurance company's computer system.
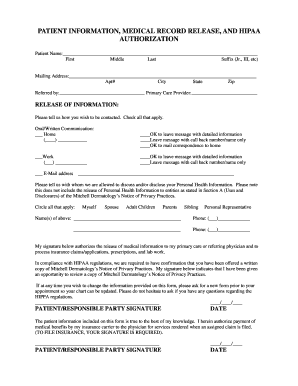
What information does HIPAA require on the release of information form?
A HIPAA-compliant HIPAA release form must, at the very least, contain the following information: A description of the information that will be used/disclosed. The purpose for which the information will be disclosed. The name of the person or entity to whom the information will be disclosed.
Why is HIPAA important summary?
HIPAA is important because it ensures healthcare providers, health plans, healthcare clearinghouses, and business associates of HIPAA-covered entities must implement multiple safeguards to protect sensitive personal and health information.
What patient information is protected by HIPAA?
Health information such as diagnoses, treatment information, medical test results, and prescription information are considered protected health information under HIPAA, as are national identification numbers and demographic information such as birth dates, gender, ethnicity, and contact and emergency contact ...
What are the 3 rules of HIPAA?
The three HIPAA rulesThe Privacy Rule.Thee Security Rule.The Breach Notification Rule.
What should a release of information include?
Recorded the date and time the request was received. Identified the date and time the requested information was needed. Identified to whom the information was to be sent. Confirmed that the request included a valid authorization.
What does release of information include?
Release of information means a written authorization, dated and signed by a client or a client's legal representative, that allows a licensee to provide specified treatment information to the individual or individuals designated in the written release of information.
What is a HIPAA disclosure?
Disclosure: Release, transfer, provisions of, access to, or divulgence in any manner of. information outside the entity holding the information. Electronic Protected Health Information: Protected health information (PHI) created, maintained or transmitted in electronic form (ePHI).
What are the 4 main rules of HIPAA?
The HIPAA Security Rule Standards and Implementation Specifications has four major sections, created to identify relevant security safeguards that help achieve compliance: 1) Physical; 2) Administrative; 3) Technical, and 4) Policies, Procedures, and Documentation Requirements.
What are the 5 Rules of HIPAA?
HHS initiated 5 rules to enforce Administrative Simplification: (1) Privacy Rule, (2) Transactions and Code Sets Rule, (3) Security Rule, (4) Unique Identifiers Rule, and (5) Enforcement Rule.
What are the 4 main purpose of HIPAA?
The HIPAA legislation had four primary objectives: Assure health insurance portability by eliminating job-lock due to pre-existing medical conditions. Reduce healthcare fraud and abuse. Enforce standards for health information. Guarantee security and privacy of health information.
What is the summary of the HIPAA Privacy Rule?
This is a summary of key elements of the Privacy Rule including who is covered, what information is protected, and how protected health information can be used and disclosed. Because it is an overview of the Privacy Rule, it does not address every detail of each provision. Summary of the Privacy Rule PDF - PDF.
When was HIPAA enacted?
Statutory and Regulatory Background. The Health Insurance Portability and Accountability Act of 1996 (HIPAA), Public Law 104-191, was enacted on August 21, 1996. Sections 261 through 264 of HIPAA require the Secretary of HHS to publicize standards for the electronic exchange, privacy and security of health information.
What is a health care clearinghouse?
Health Care Clearinghouses.Health care clearinghouses are entities that process nonstandard information they receive from another entity into a standard (i.e., standard format or data content), or vice versa. 7 In most instances, health care clearinghouses will receive individually identifiable health information only when they are providing these processing services to a health plan or health care provider as a business associate. In such instances, only certain provisions of the Privacy Rule are applicable to the health care clearinghouse’s uses and disclosures of protected health information. 8 Health care clearinghouses include billing services, repricing companies, community health management information systems, and value-added networks and switches if these entities perform clearinghouse functions.
What is protected health information?
The Privacy Rule protects all "individually identifiable health information" held or transmitted by a covered entity or its business associate, in any form or media, whether electronic , paper , or oral. The Privacy Rule calls this information "protected health information (PHI).".
What is the purpose of the Privacy Rule?
A major goal of the Privacy Rule is to assure that individuals’ health information is properly protected while allowing the flow of health information needed to provide and promote high quality health care and to protect the public's health and well being.
How often do health plans have to give privacy notice?
Thereafter, the health plan must give its notice to each new enrollee at enrollment, and send a reminder to every enrollee at least once every three years that the notice is available upon request.
When was the Privacy Rule published?
The Department received over 52,000 public comments. The final regulation, the Privacy Rule, was published December 28, 2000. 2. In March 2002, the Department proposed and released for public comment modifications to the Privacy Rule.
What is HIPAA law?
It may seem strange, but the answers to these questions lie in the Health Insurance Portability and Accountability Act of 1996 (HIPAA). HIPAA applies not only to health insurance but privacy and medical records issues as well.
What is the act that regulates how our health information is handled to protect our privacy?
HIPAA, the same act that regulates how our health information is handled to protect our privacy, also gives us the right to see and obtain a copy of our records and to dispute anything we feel is erroneous or has been omitted. 1
How long does it take to get a copy of your medical records?
2 In most cases, the copy must be provided to you within 30 days.
What to do if you find an error in your medical records?
If you find an error in your medical records, you can request that it be corrected. You can also ask them to add information to your file if it's incomplete or change something you disagree with. For example, if you and your doctor agree that there's an error such as what medication was prescribed, they must change it.
Why are medical records important?
Our medical records are vitally important for a number of reasons. They're the way your current doctors follow your health and health care. They provide background to specialists and bring new doctors up-to-speed. Your medical records are the records of the people with whom we literally entrust our lives. While you have certain rights regarding ...
How long does it take to change a doctor's record?
In most cases, the file should be changed within 60 days, but it can take an additional 30 days if you're given a reason. 4 .
Can you get all your medical information?
In a few special cases, you may not be able to get all of your information. For example, if your healthcare provider decides something in your file might endanger you or someone else, they may not have to give you that information.
What is HIPAA protected health information?
The HIPAA Privacy Rule protects the privacy of individually identifiable health information, called protected health information (PHI), as explained in the Privacy Rule and here - PDF - PDF. The Security Rule protects a subset of information covered by the Privacy Rule, which is all individually identifiable ...
What was the HIPAA prior to?
Prior to HIPAA, no generally accepted set of security standards or general requirements for protecting health information existed in the health care industry. At the same time, new technologies were evolving, and the health care industry began to move away from paper processes and rely more heavily on the use of electronic information systems to pay claims, answer eligibility questions, provide health information and conduct a host of other administrative and clinically based functions.
What is the HIPAA Privacy and Security Rule?
1 To fulfill this requirement, HHS published what are commonly known as the HIPAA Privacy Rule and the HIPAA Security Rule. The Privacy Rule, or Standards for Privacy of Individually Identifiable Health Information, establishes national standards for the protection of certain health information. The Security Standards for the Protection of Electronic Protected Health Information (the Security Rule) establish a national set of security standards for protecting certain health information that is held or transferred in electronic form. The Security Rule operationalizes the protections contained in the Privacy Rule by addressing the technical and non-technical safeguards that organizations called “covered entities” must put in place to secure individuals’ “electronic protected health information” (e-PHI). Within HHS, the Office for Civil Rights (OCR) has responsibility for enforcing the Privacy and Security Rules with voluntary compliance activities and civil money penalties.
What is the summary of the HIPAA security rule?
This is a summary of key elements of the Security Rule including who is covered, what information is protected, and what safeguards must be in place to ensure appropriate protection of electronic protected health information. Because it is an overview of the Security Rule, it does not address every detail ...
What is the HITECH Act?
The HITECH Act of 2009 expanded the responsibilities of business associates under the HIPAA Security Rule. HHS developed regulations to implement and clarify these changes. See additional guidance on business associates.
What is the Privacy Rule?
The Privacy Rule, or Standards for Privacy of Individually Identifiable Health Information, establishes national standards for the protection of certain health information. The Security Standards for the Protection of Electronic Protected Health Information (the Security Rule) establish a national set of security standards for protecting certain ...
Why are risk analysis and management provisions of the Security Rule addressed separately?
The risk analysis and management provisions of the Security Rule are addressed separately here because, by helping to determine which security measures are reasonable and appropriate for a particular covered entity, risk analysis affects the implementation of all of the safeguards contained in the Security Rule.
What is the HIPAA Privacy Rule?
The HIPAA Privacy Rule establishes national standards to protect individuals' medical records and other personal health information and applies to health plans, health care clearinghouses, and those health care providers that conduct certain health care transactions electronically. The Rule requires appropriate safeguards to protect the privacy of personal health information, and sets limits and conditions on the uses and disclosures that may be made of such information without patient authorization. The Rule also gives patients rights over their health information, including rights to examine and obtain a copy of their health records, and to request corrections.
Where is the Privacy Rule located?
The Privacy Rule is located at 45 CFR Part 160 and Subparts A and E of Part 164 .
Who has the right to access your medical records?
Access. Only you or your personal representative has the right to access your records. A health care provider or health plan may send copies of your records to another provider or health plan only as needed for treatment or payment or with your permission.
What to do if your medical record is incorrect?
Corrections. If you think the information in your medical or billing record is incorrect, you can request a change, or amendment, to your record. The health care provider or health plan must respond to your request. If it created the information, it must amend inaccurate or incomplete information.
What is a psychotherapy note?
Psychotherapy notes are notes that a mental health professional takes during a conversation with a patient. They are kept separate from the patient’s medical and billing records. HIPAA also does not allow the provider to make most disclosures about psychotherapy notes about you without your authorization.
What is the privacy rule?
The Privacy Rule gives you, with few exceptions, the right to inspect, review, and receive a copy of your medical records and billing records that are held by health plans and health care providers covered by the Privacy Rule.
What happens if a provider does not agree to your request?
If the provider or plan does not agree to your request, you have the right to submit a statement of disagreement that the provider or plan must add to your record.
Can a provider deny you a copy of your records?
A provider cannot deny you a copy of your records because you have not paid for the services you have received. However, a provider may charge for the reasonable costs for copying and mailing the records. The provider cannot charge you a fee for searching for or retrieving your records.
Does HIPAA require health care providers to share information with other providers?
The Privacy Rule does not require the health care provider or health plan to share information with other providers or plans. HIPAA gives you important rights to access - PDF your medical record and to keep your information private.
What are HIPAA regulations for medical records?
HIPAA regulations for medical records dictate the mandatory data storage and release policies that all healthcare institutions have to comply with. As a federal law, HIPAA is governed by the Department of Health and Human Services (HHS). However, the HIPAA regulations for medical records retention and release may differ in different states.
What is the HIPAA Security Rule?
The protection of ePHI comes under the HIPAA Security Rule – a modern HIPAA addendum that was established to address the continuously evolving medical technology and growing trend of saving PHI information electronically.
What happens if you fail to provide patient records?
Failure to provide patient records can result in a HIPAA fine.
What is protected health information?
Protected Health Information (PHI) is a broad term that is used to denote the patients’ identifiable information (PII) including; name, address, age, sex, and other health0related data which is generally collected and stored by medical practitioners using specialized medical software.
How long do hospitals keep medical records in Oregon?
According to Oregon HIPPA medical records release laws, hospitals are required to keep the medical records of patients for 10 years after the date of last discharge.
How long do doctors have to hold patient data in Florida?
Medical doctors in Florida are required to hold patients’ data for the last 5 years
How long do you have to keep medical records in Texas?
For adult patients, hospitals in Texas are required to keep the medical records for 10 years from the date of last treatment.
Who is responsible for HIPAA?
The HIPAA regulations are policed by the U.S. Department of Health & Human Services’ Office for Civil Rights (OCR). State Attorneys General can also take action against Covered Entities and Business Associates found not to be in compliance with HIPAA.
How long do you have to keep HIPAA records?
CFR §164.316 (b) (2) (i) states that HIPAA-related documents must be retained for a period of six years from the date that the document was created. For policies, it is six years from when the policy was last in effect. Insurance companies may be subject to FINRA laws which cover the retention of certain records.
Who does HIPAA apply to?
Practically all health plans, healthcare clearinghouses, healthcare providers and endorsed sponsors of the Medicare prescription drug discount card are considered to be “HIPAA Covered Entities” (CEs) under the Act. Normally, these are entities that come into contact with PHI on a constant basis.
What is the HIPAA Privacy Rule?
HIPAA Privacy Rule: The Privacy Rule dictates how, when and under what circumstances PHI can be used and disclosed. Enacted for the first time in 2003, it applies to all healthcare organizations, clearinghouses and entities that provide health plans.
What is the HIPAA breach notification rule?
The HIPAA Breach Notification Rule – 45 CFR §§ 164.400-414 – requires notifications to be issued after a breach of unsecured protected health information.
What are the violations of HIPAA?
Violations of HIPAA often result from the following: 1 Lack of adequate risk analyses. 2 Lack of comprehensive employee training. 3 Inadequate Business Associate Agreements. 4 Inappropriate disclosures of PHI. 5 Ignorance of the minimum necessary rule. 6 Failure to report breaches within the prescribed timeframe.
How many personal identifiers are there in HIPAA?
For the benefit of clarification, we have detailed below the eighteen personal identifiers that could allow a person to be identified. In the context of HIPAA for Dummies, when these personal identifiers are combined with health data the information is known as “Protected Health Information” or “PHI”. When stored or communicated electronically, the acronym “PHI” is preceded by an “e” – i.e. “ePHI”.
What is a HIPAA document?
a document that include the HIPAA standards or requirements
What is HIPAA billing?
under HIPAA, terms that provide for uniformity and simplification of health care billing and record keeping
What does "limited amount of patient information" mean?
Term referring to the limited amount of patient information that may be disclosed, depending on circumstances.
Is a patient's medical record considered property?
Patients' medical records are considered the property of the owners of the facility where they were created
What are the rights of a patient under HIPAA?
Under the HIPAA Privacy Rule, patients have several rights regarding their medical records, including a right to access, a right to amend, and, in some circumstances, a right to restrict disclosures of their protected health information (PHI). Understanding and complying with those rights is an important component of quality patient care.
What is the HIPAA Privacy Rule?
PHI used for marketing purposes and for purposes beyond what is allowed by the HIPAA Privacy Rule (i.e., treatment, payment, or healthcare operations) require the patient’s advance written authorization. A PT provider was fined $25,000 for using a patient’s PHI for marketing without consent. The provider was not only fined for posting PHI on the clinic’s website without authorization, but also for failing to reasonably safeguard PHI and implement written policies protecting PHI.
How long do you have to keep a signed authorization?
The provider must supply the patient with a copy of the signed authorization and retain all signed authorization forms for six years from either the date of the form’s creation or the date when it was last in effect, whichever is later. For more resources on creating and verifying a valid authorization, see this HHS decision tool. And here is a sample authorization form you can use as an example for building your form.
What is the purpose of a written request?
Make sure the purpose of your written request process is to track and validate the patient’s request and not to create a barrier for access. Consider options such as email requests; a webform on your website that the patient can complete online; and forms that request just basic information (e.g., patient name and address).
What is a physician name?
The name or other specific identification of the person (s) or class of persons authorized to make the requested use or disclosure (e.g., physician name, practice name).
What is right of access in healthcare?
Keep in mind: Right of Access is based on the concept that patients’ ability to access their records is empowering and engages them in their own health care. PTs, OTs, and SLPs are all about engaging and empowering the patient, so providing a streamlined, efficient process for patients to access their records is more about providing good patient care than merely checking a compliance box.
What is the signature of a patient?
Signature of the patient, date, and—if the authorization is signed by a personal representative of the patient—a description of the representative’s authority to act for the patient.
Treatment
Definition
Activities
- Health care operations are any of the following activities: (a) quality assessment and improvement activities, including case management and care coordination; (b) competency assurance activities, including provider or health plan performance evaluation, credentialing, and accreditation; (c) conducting or arranging for medical reviews, audits, or legal services, includin…
Resources
- Public Health Activities. Covered entities may disclose protected health information to: (1) public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability and to public health or other government authorities authorized to receive reports of child abuse and neglect; (2) entities subject to FDA regulation re…
Scope
- Victims of Abuse, Neglect or Domestic Violence. In certain circumstances, covered entities may disclose protected health information to appropriate government authorities regarding victims of abuse, neglect, or domestic violence.31 Health Oversight Activities. Covered entities may disclose protected health information to health oversight agencies (as defined in the Rule) for purposes o…
Purpose
- Law Enforcement Purposes. Covered entities may disclose protected health information to law enforcement officials for law enforcement purposes under the following six circumstances, and subject to specified conditions: (1) as required by law (including court orders, court-ordered warrants, subpoenas) and administrative requests; (2) to identify or ...
Uses
- Cadaveric Organ, Eye, or Tissue Donation. Covered entities may use or disclose protected health information to facilitate the donation and transplantation of cadaveric organs, eyes, and tissue.36
Introduction
- Research. Research is any systematic investigation designed to develop or contribute to generalizable knowledge.37 The Privacy Rule permits a covered entity to use and disclose protected health information for research purposes, without an individuals authorization, provided the covered entity obtains either: (1) documentation that an alteration or waiver of individuals au…
Functions
- Essential Government Functions. An authorization is not required to use or disclose protected health information for certain essential government functions. Such functions include: assuring proper execution of a military mission, conducting intelligence and national security activities that are authorized by law, providing protective services to the President, making medical suitability …
Advantages
- The covered entities in an organized health care arrangement may use a joint privacy practices notice, as long as each agrees to abide by the notice content with respect to the protected health information created or received in connection with participation in the arrangement.53 Distribution of a joint notice by any covered entity participating in the organized health care arra…
Operation
- A health plan must distribute its privacy practices notice to each of its enrollees by its Privacy Rule compliance date. Thereafter, the health plan must give its notice to each new enrollee at enrollment, and send a reminder to every enrollee at least once every three years that the notice is available upon request. A health plan satisfies its distribution obligation by furnishing the notice …
Popular Posts:
- 1. grassy pond family medicine/patient portal
- 2. alaska family care associates patient portal
- 3. sghs patient portal
- 4. when providing a patient report via radio
- 5. patient portal manakto mayo
- 6. amh patient portal, auburn memorial
- 7. urology patient portal auburn al
- 8. horizon lssrr vision patient portal
- 9. planned parenthood patient portal pottstown pa
- 10. dr james reidy patient portal