Patient Portals and the HIPAA Security Rule - Compliancy …
2 hours ago · Patient Portals and the HIPAA Security Rule. Healthcare providers frequently allow patients to access their electronic health records (EHRs) through a patient portal. Online patient portals allow patients to view their medical records, schedule appointments, and even request refills of prescriptions, anywhere the patient has access to the Internet. Patient portals contain … >> Go To The Portal
What are the patients rights under HIPAA?
· Patient Portals and the HIPAA Security Rule. Healthcare providers frequently allow patients to access their electronic health records (EHRs) through a patient portal. Online patient portals allow patients to view their medical records, schedule appointments, and even request refills of prescriptions, anywhere the patient has access to the Internet. Patient portals contain …
What are the rules of HIPAA?
For those covered entities providing individuals with access to their PHI through web portals, those portals should already be set up with appropriate authentication controls, as required by 45 CFR 164.312 (d) of the HIPAA Security Rule, to ensure that the person seeking access is the individual or the individual’s personal representative.
What is a patient portal?
Those who may access the portal could include the following: The individual (patient or client). An authorized person, as permitted by a HIPAA-compliant authorization. A designee that the individual designates in writing. A personal representative. A personal representative―that is, …
Are patient portals required?
· Ensure a HIPAA expert audits the final patient portal. Have your terms and conditions created/reviewed by an attorney that specializes in HIPAA law. Require patients log in each time to access PHI, with a 30-minute auto-logout. To make the patient portal more convenient and user-friendly, consider using face or fingerprint recognition for logins.

What does HIPAA have to say about patient portals?
Online patient portals allow patients to view their medical records, schedule appointments, and even request refills of prescriptions, anywhere the patient has access to the Internet. Patient portals contain information that constitutes electronic protected health information (ePHI) under the HIPAA Security Rule.
Are patient portals HIPAA compliant?
HIPAA Compliance and Healthcare Portals So, are healthcare portals HIPAA compliant? The short answer is yes, they are and must be. But, let's talk about what that means specifically for you as a provider. Under HIPAA regulations, your practice is required to make protecting patients' medical data a priority.
Are patient portals confidential?
Yes, many patient portals are secure as they have security and privacy safeguards to keep your information protected. To ensure your data remains protected from any unauthorized access, these healthcare portals are hosted on a secure connection and can be accessed via a password-protected login.
What safeguards are included in patient portals?
Patient portals have privacy and security safeguards in place to protect your health information. To make sure that your private health information is safe from unauthorized access, patient portals are hosted on a secure connection and accessed via an encrypted, password-protected logon.
Is Facebook portal HIPAA compliant?
Conclusion: Facebook is not HIPAA compliant because it will not sign a BAA. However, covered entities can use it—as long as they do not share any PHI.
What are disadvantages of patient portals?
Even though they should improve communication, there are also disadvantages to patient portals....Table of ContentsGetting Patients to Opt-In.Security Concerns.User Confusion.Alienation and Health Disparities.Extra Work for the Provider.Conclusion.
What are the pros and cons of using a patient portal?
What are the Top Pros and Cons of Adopting Patient Portals?Pro: Better communication with chronically ill patients.Con: Healthcare data security concerns.Pro: More complete and accurate patient information.Con: Difficult patient buy-in.Pro: Increased patient ownership of their own care.
Should patients have access to their medical records?
The studies revealed that patients' access to medical records can be beneficial for both patients and doctors, since it enhances communication between them whilst helping patients to better understand their health condition. The drawbacks (for instance causing confusion and anxiety to patients) seem to be minimal.
What are the benefits of a patient portal?
What are the benefits of patient portals?Patient portals are efficient. ... Patient portals improve communication. ... They store health information in one place. ... Patient portals satisfy meaningful use standards. ... They improve data accuracy. ... Patient portals make refilling prescriptions easy. ... They're available whenever you need them.More items...•
What makes the patient portal different from a PHR?
Patient portals are distinct from PHRs because they are tethered to the clinician-facing EHR. Most EHR vendors sell patient portals as a part of the overall software suite, and patient portals came to prominence as a part of meaningful use requirements.
Why are patient portals so important?
The Benefits of a Patient Portal You can access all of your personal health information from all of your providers in one place. If you have a team of providers, or see specialists regularly, they can all post results and reminders in a portal. Providers can see what other treatments and advice you are getting.
What is the HIPAA Privacy Rule?
With limited exceptions, the HIPAA Privacy Rule (the Privacy Rule) provides individuals with a legal, enforceable right to see and receive copies upon request of the information in their medical and other health records maintained by their health care providers and health plans.
Who has the right to access health records?
The Privacy Rule generally also gives the right to access the individual’s health records to a personal representative of the individual. Under the Rule, an individual’s personal representative is someone authorized under State or other applicable law to act on behalf of the individual in making health care related decisions. With respect to deceased individuals, the individual’s personal representative is an executor, administrator, or other person who has authority under State or other law to act on behalf of the deceased individual or the individual’s estate. Thus, whether a family member or other person is a personal representative of the individual, and therefore has a right to access the individual’s PHI under the Privacy Rule, generally depends on whether that person has authority under State law to act on behalf of the individual. See 45 CFR 164.502 (g) and 45 CFR 164.524.
How long does a covered entity have to respond to a HIPAA request?
Under the HIPAA Privacy Rule, a covered entity must act on an individual’s request for access no later than 30 calendar days after receipt of the request. If the covered entity is not able to act within this timeframe, the entity may have up to an additional 30 calendar days, as long as it provides the individual – within that initial 30-day period – with a written statement of the reasons for the delay and the date by which the entity will complete its action on the request. See 45 CFR 164.524 (b) (2).
How long does it take to respond to a PHI request?
In providing access to the individual, a covered entity must provide access to the PHI requested, in whole, or in part (if certain access may be denied as explained below), no later than 30 calendar days from receiving the individual’s request. See 45 CFR 164.524 (b) (2). The 30 calendar days is an outer limit and covered entities are encouraged to respond as soon as possible. Indeed, a covered entity may have the capacity to provide individuals with almost instantaneous or very prompt electronic access to the PHI requested through personal health records, web portals, or similar electronic means. Further, individuals may reasonably expect a covered entity to be able to respond in a much faster timeframe when the covered entity is using health information technology in its day to day operations.
How long does it take to get access to a certified EHR?
While the Privacy Rule permits a covered entity to take up to 30 calendar days from receipt of a request to provide access (with one extension for up to an additional 30 calendar days when necessary), covered entities are strongly encouraged to provide individuals with access to their health information much sooner, and to take advantage of technologies that enable individuals to have faster or even immediate access to the information.
What is access requested?
The access requested is reasonably likely to cause substantial harm to a person (other than a health care provider) referenced in the PHI. The provision of access to a personal representative of the individual that requests such access is reasonably likely to cause substantial harm to the individual or another person.
What are the two categories of information that are expressly excluded from the right of access?
In addition, two categories of information are expressly excluded from the right of access: Psychotherapy notes , which are the personal notes of a mental health care provider documenting or analyzing the contents of a counseling session, that are maintained separate from the rest of the patient’s medical record.
What are the privacy concerns of patient portals?
The main privacy issues involve the aforementioned patient right of access and their right to request correction and/or amendment.
How to keep HIPAA compliance documentation?
Jon included tabs in the three-ring binder for everything that you need to document and a checklist for each tab. I recommend adding the date that you check off each item in each checklist, as one of our clients suggested to us.
Why are portals important?
Allowing patients to make appointments themselves on the portal and request medication refills helps streamline otherwise time-consuming tasks. Improve communications.
What is access likely to endanger?
The access is reasonably likely to endanger the life or physical safety of the individual or another.
What is family access?
Provide access to family members to perform functions on behalf of the patient.
Is the patient portal a form?
The patient portal will not be every patient’s requested form or format. Thus, the covered entity must continue to provide alternatives, such as hard copies, CDs, or email attachments.
Does HIPAA require a hard copy?
Other than the access issue raised above, generally speaking, HIPAA provides that individuals are entitled to a copy in the form or format that they request, if readily producible. If not readily producible, the covered entity’s default is to produce a hard copy or an electronic copy, depending on whether it maintains the requested protected health information (“PHI”) electronically.
What is a HIPAA patient portal?
A HIPAA Patient Portal is a form of patient engagement in which health care providers can share information with a patient. If said information includes PHI and medical records, the patient portal must be HIPAA compliant.
What is HIPAA Privacy?
What Is HIPAA? The Health Insurance Portability and Accountability Act (HIPAA) protects patients’ privacy by limiting access to PHI (Protected Health Information) and governing acceptable use of their health data. The HIPAA Privacy Rule is composed of national regulations for the use and disclosure of PHI in healthcare treatment, payment, ...
What is a BAA in healthcare?
When working with a web design, hosting company, patient portal vendor, or healthcare app development company, always get a BAA (Business Associate Agreement). A BAA shares the responsibility for all patient information that is received by the company or handled by the patient portal they build.
How much is an EPHI violation fine?
A covered entity that did not know and could not have reasonably known of an ePHI breach could be fined $100-$50,000 per incident and up to $1.5 Million.
What are the controls for access control?
Access controls must include unique user identification, emergency access procedure, and automatic logoff. According to HIPAA, the information in a medical patient portal should be encrypted at all times – at rest and in transit.
How long does it take to log out of PHI?
Require patients log in each time to access PHI, with a 30-minute auto-logout. To make the patient portal more convenient and user-friendly, consider using face or fingerprint recognition for logins.
What is protected health information?
Protected Health Information (PHI) is any information that is held by a covered entity regarding a patient’s health status, provision of health care, or health care payment.
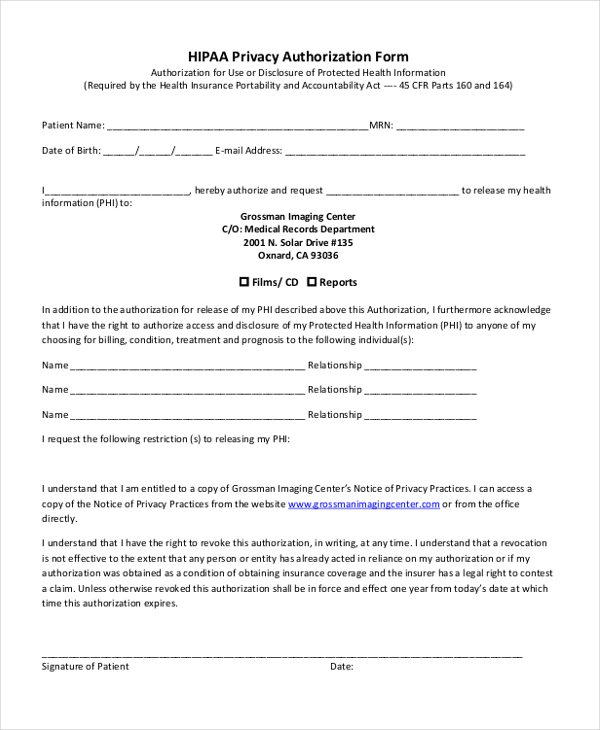
How to request records from a patient?
To request records, a patient needs to contact their provider’s health information management (HIM) department, the post explained. The individual will then need to complete a “Patient Access Request (or similarly titled)” form.
Can a power of attorney access a patient's medical records?
Furthermore, if an individual was given power of attorney for a patient, then he or she has the right to request access to another person’s medical records.
Is patient access to their own information a right under HIPAA?
However, patient data access is often misunderstood, and individuals can be unaware of what information they are able to obtain from their provider.
Can HIPAA charge for copies of health information?
There are also permissible fees that covered entities can charge an individual for copies of their own health information . HIPAA entities can calculate their own fees, even for ePHI requests, as long as it is within the limits of HIPAA’s Privacy Rule.
Can a patient's personal representative make a decision on behalf of the patient?
It is important to note that HIPAA regulations also allow for a patient’s personal representative to complete patient access requests in the place of a patient. These representatives are allowed to make healthcare decisions on the patient’s behalf under state law.
Is it beneficial to access patients' own data?
The AHIMA post underlined the potential benefits of patients accessing their own data, saying that it could be beneficial if an individual is transferring to a new provider.
Can a HIPAA covered provider refuse access to a patient's medical records?
A HIPAA covered health plan or provider can refuse access only in very limited circumstances. Additionally, patients have access to data including laboratory results, images, prescription history, physician notes, diagnoses, and similar information. “When individuals get, review, use and share copies of their health information, ...
What is privacy and security?
Building privacy and security protections into technology products enhances their value by providing some assurance to users that the information is secure and will be used and disclosed only as approved or expected. Such protections are sometimes required by federal and state laws, including the HIPAA Privacy, Security, ...
What is OCR in health?
OCR offers guidance to mobile health (mHealth) developers and others interested in the intersection of health information technology and HIPAA privacy and security protections.
What is the HIPAA Privacy Rule?
The HIPAA Privacy Rule allows covered entities and business associates to charge a fee, and states that organizations can calculate their own price.
What is the potential back and forth between paper and electronic records?
The potential back and forth between paper and electronic records was listed as a possible drawback to patient data access.
What are the challenges of implementing HIPAA compliant patient portals?
The challenges of implementing HIPAA compliant patient portals depend on a provider's IT infrastructure and its operating system's complexity and interoperability. There are also the legal and regulatory requirements that include meeting mandatory HIPAA guidelines and voluntary best practices. The challenges of HIPAA compliant portal development include:
What are patient portals?
Patient portals generate many associated mandatory and medical compliance issues. Practices must consider their business associates and chain-of-trust issues that arise when sending information by electronic transmission. Medical companies deal with insurance companies, Internet service providers, labs, pharmacies, billing and coding services, hospitals and other practices across different medical-related specialties.
What are the challenges of HIPAA?
The challenges of implementing HIPAA compliant patient portals depend on a provider's IT infrastructure and its operating system's complexity and interoperability. HIPAA regulations also provide legal and regulatory requirements that include meeting mandatory HIPAA guidelines and voluntary best practices. Here are the most common challenges that occur during HIPAA compliant portal development.
What is HIPAA eCommerce?
HIPAA eCommerce platforms provide patient portals that streamline workflow, free staff members from routine clerical work, reduce operating costs, and strengthen patient loyalty to their health care providers. Although some patients have been reluctant to use patient portals, statistics show that patients want the ability to access their records online. [1] IT vendor athenahealth conducted comprehensive studies of patient portal use based on 3,500 medical groups and 7.5 million patients. The insights that this research provided include:
What is the HIPAA Privacy Rule?
The HIPAA Privacy Rule gives patients the right to obtain copies of their medical records, treatments and protected health information or PHI. These requirements go further if medical providers want to receive reimbursement from Medicare and Medicaid -- patients must be able to access their records online, download copies and transmit the information to third-party providers. Most medical practices are finding it necessary to develop patient portals where patients and physicians can interact, share information and perform important functions such as practices billing patients and accepting payments online. HIPAA standards rule requires that these patient portals have strong security and privacy protections to prevent unauthorized access of these confidential PHI records.
What stakeholders are involved in developing a patient portal?
These include the practice's senior leadership, patient advocates in the community, risk management stakeholders like insurers and legal counsel, physicians and clinicians and marketing staffs and health information management professionals who need to sell the benefits of using the patient portal to patients, caregivers and even some staff members who might hesitate to interact with patients electronically. Patient portals enhance communications, and sounding out these stakeholders is essential for developing an effective portal because each will be using the technology at ever-increasing rates.
What is the effect of patient portal adoption?
Patient portal adoption increases patient payments and reduces the amounts that health providers send to collections.
Popular Posts:
- 1. patient site bidmc login
- 2. northside medical patient portal
- 3. conway medical center patient portal sign up
- 4. southeastern patient portal in tallahassee fl
- 5. grays harbor community hospital patient portal
- 6. patient portal chicago family health center
- 7. 7 days pediatrics patient portal
- 8. covenant patient portal waterloo iowa
- 9. my fresenius patient hub
- 10. maine integrative tetzlaff patient portal