Guidelines for Perioperative Practice - Clinical Resources ...
26 hours ago Guidelines for Perioperative Practice. AORN is committed to promoting excellence in perioperative nursing practice, advancing the profession, and supporting the professional … >> Go To The Portal
Does this update address the perioperative management of the patient without implantable devices?
This update does not address the perioperative management of the patient without a cardiac implantable electronic device, such as those (1) with only a temporary cardiac implantable electronic device; (2) with only a noncardiac implantable device (e. g.
Why adhere to the AORN guidelines for Perioperative Practice?
When adhering to the AORN Guidelines for Perioperative Practice, perioperative clinicians can be confident that they are following trustworthy guidelines developed in accordance with the principles set forth by the National Academy of Medicine. 1
What is the OTN's experience of responsibility in Perioperative Practice?
RESULTS The results revealed the OTN's experiences of responsibility for patient's care in perioperative practice as two main themes: “the formal external responsibility” and “personal ethical value”.
Is there a need for a UK wide perioperative risk assessment system?
A review of the perioperative care of surgical patients This report, released by NCEPOD in 2011, recommends that: There is a need to introduce a UK wide system that allows rapid and easy identification of patients who are at high risk of postoperative mortality and morbidity. (Departments of Health in England, Wales & Northern Ireland)
What is included in a preoperative assessment?
A pre-operative physical examination is generally performed upon the request of a surgeon to ensure that a patient is healthy enough to safely undergo anesthesia and surgery. This evaluation usually includes a physical examination, cardiac evaluation, lung function assessment, and appropriate laboratory tests.
What is ASA guideline?
The ASA physical status classification system, which is based upon the patient's physical health status, is used by physicians (anesthesiologists, surgeons) to predict anesthetic and surgical risk prior to a procedure. Practice Guidelines. ASA physical status classification is documented for each patient.
What is the ASA?
American Society of Anesthesiologists (ASA)
What is required for pre op clearance?
A history and physical examination, focusing on risk factors for cardiac, pulmonary and infectious complications, and a determination of a patient's functional capacity, are essential to any preoperative evaluation.
What does ASA 3 mean?
ASA 3: A patient with a severe systemic disease that is not life-threatening.
What does ASA 4 mean?
ASA IV. A patient with severe systemic disease with constant threat to life, as follows: Heart attack less than 3 months ago.
What is an ASA assessment?
The ASA score is a subjective assessment of a patient's overall health that is based on five classes (I to V). Patient is a completely healthy fit patient. Patient has mild systemic disease. Patient has severe systemic disease that is not incapacitating.
Who determines ASA classification?
While the Physical Status classification may initially be determined at various times during the preoperative assessment of the patient, the final assignment of Physical Status classification is made on the day of anesthesia care by the anesthesiologist after evaluating the patient.
What does the ASA cover?
Radio and TV ads (including teleshopping presentations) Ads on the internet, smartphones and tablets. Ad claims on companies' own websites. Commercial e-mail and text messages.
What are the steps in pre-operative preparation?
The preoperative preparations include the following:Medical history and physical examination. ... Laboratory tests. ... Blood type and crossmatch. ... Chest x-ray. ... Electrocardiogram (ECG). ... Diagnostic procedures. ... Written instructions. ... Informed consent.More items...•
What are three things you should always ask a patient before surgery?
10 Questions to Ask before Having an OperationWhy do I need this operation?How will the operation be performed?Are there other treatment options, and is this operation the best option for me?What are the risks, benefits, and possible complications for this operation? ... What are my anesthesia options?More items...
Why is patient history important before surgery?
Preoperative education not only prepares the patient for surgery but also prepares them for what to expect following the surgery.
What is the guidance report on prehabilitation?
The guidance report, Prehabilitation for people with cancer , promotes evidence that when services are redesigned so that prehabilitation is integrated into the cancer pathway: patients feel empowered and quality of life is improved. physical and psychological resilience to cancer treatments is maximised.
What is GPAS in healthcare?
The Guidelines for the Provision of Anaesthetic Services (GPAS) support anaesthetists with responsibilities for service delivery and healthcare managers to design and deliver high quality anaesthetic services. It is developed using a rigorous, evidence-based process, which was accredited by the National Institute for Health and Care Excellence (NICE) in 2016.
What is CF guidance?
The guidance aims to provide a background knowledge of Cystic Fibrosis [CF] for the anaesthetist and give guidance and best practice for the perioperative anaesthetic management of the patient with CF presenting for surgery.
Is CF a high risk group for anaesthesia?
Therefore CF patients are generally considered a high risk group for anaesthesia, particularly given their potential for postoperative respiratory complications.
Is it mandatory to apply the recommendations?
It is not mandatory to apply the recommendations, and the guideline does not override the responsibility to make decisions appropriate to the circumstances of the individual, in consultation with them and their families and carers or guardian. Click here to read the guidelines in full.
Is GPAS a rigorous process?
It is developed using a rigorous, evidence-based process, which was accredited by the National Institute for Health and Care Excellence (NICE) in 2016. Each of the GPAS chapters should be seen as independent but interlinked documents.
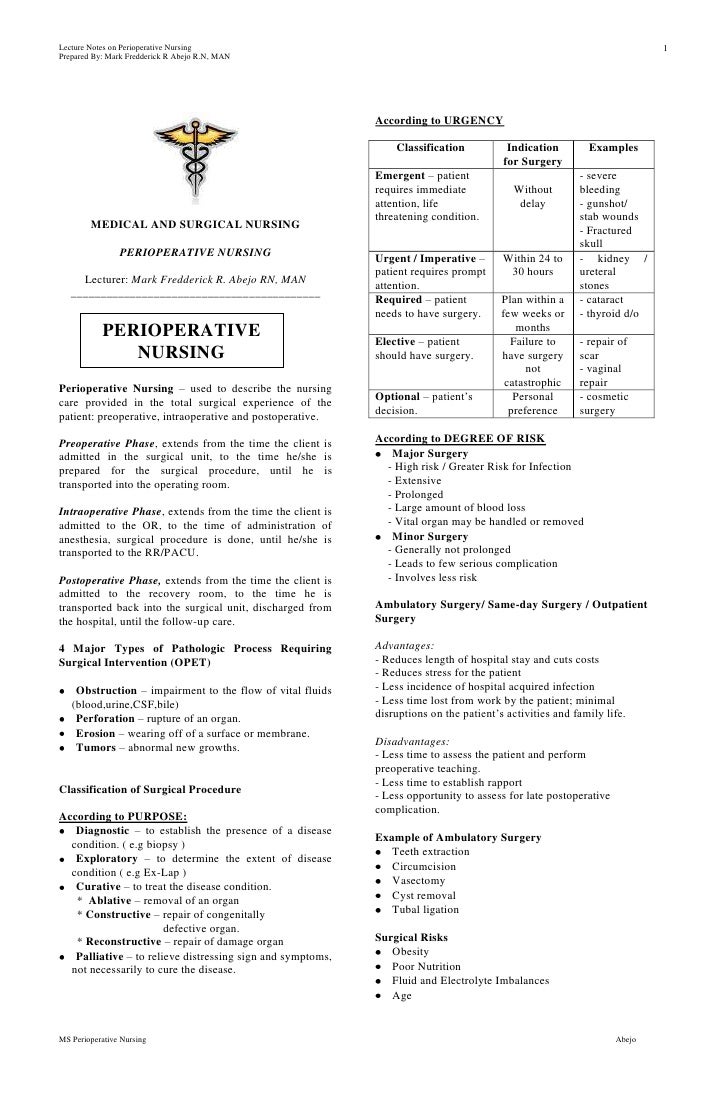
What is perioperative nursing?
Lindwall and von Post (2008) described perioperative nursing in relation to Swedish conditions and the text was revised by Lindwall and Blomberg (2018) as: “Perioperative nursing is a nurse anaesthetists” and operating theatre nurses' pre‐, intra‐ and postoperative care for a patient who is undergoing surgery. Perioperative nursing includes all nursing activities related to the surgical treatments, organization and leadership of the perioperative practice. Perioperative dialogues are nurse anaesthetists' and operating theatre nurse's pre‐, intra‐ and postoperative dialogues with the patient, with the purpose to plan, implement and evaluate perioperative nursing and create continuity in patient care'.
What is an OTN in perioperative practice?
In this study, we want to obtain an understanding of the operating theatre nurses' (OTNs') responsibility for patient safety and care in perioperative practice. Perioperative practice is demanding; it is complex, highly technical and very different compared with other settings. OTNs are responsible for aseptic, instrumentation, infection prevention and complication measures, medical technique, handling of biological preparations, as well as collaborating and planning care in consultation with the patient, surgical team and other healthcare providers (Gillespie & Hamlin, 2009; Kelvered, Öhlén, & Gustafsson, 2012). OTN's often work in challenging situations under a fast pace and have to address the basic concepts that are unique in ensuring the surgical patient's safety (Spruce, 2013).
Why is it my responsibility to choose the right operating table with accessories?
It is my responsibility to choose the right operating table with accessories because we know what is expected and some surgery require special X‐ray tables and they must be from the beginning… If the surgery requires more space, I need to know where the surgeon and patient's armrest are best placed. From experience we know where pressure can occur…its also up to me to find out that the patient is aware of what is planned. (#5)
How many steps were taken in the interpretation of the interviews?
3.4.1. The interpretation of the interviews was done in five steps:
Why do I cover my patient?
I always cover the patient to prevent the patient from being exposed or getting cold… even if it is an acute patient. If intimate parts have been exposed, we lower the legs and cover with a sheet before surgery is finished. I raise the temperature of the operating theatre to maintain body temperature… when the patient is protected with an electric blanket, the temperature can be lowered… but not if it is an older person who needs extra warmth. (#13)
What is perioperative management?
Perioperative management refers to the preoperative, intraoperative, postoperative, or recovery period in any setting where an anesthesia provider will be delivering anesthesia care. Adverse outcomes associated with cardiac implantable electronic device function include, but are not limited to, damage to the device, inability of the device to deliver pacing or shocks, lead-tissue interface damage, changes in pacing behavior, electrical reset to the backup pacing mode, and inappropriate implantable cardioverter–defibrillator therapies. ‡
What is preoperative preparation?
Preoperative preparation for patient safety and proper maintenance of the cardiac implantable electronic device during a planned procedure includes the following topics: (1) sources of electromagnetic interference; (2) preoperative reprogramming of the cardiac implantable electronic device’s pacing function to an asynchronous pacing mode or disabling any special algorithms, including rate adaptive pacing functions; (3) suspending the antitachyarrhythmia functions for an implantable cardioverter–defibrillator; and (4) availability of temporary pacing and defibrillation equipment.
What is a focused preoperative evaluation?
A focused preoperative evaluation of the patient with a cardiac implantable electronic device consists of the following topics: (1) determining whether a patient has a cardiac implantable electronic device; (2) determining the cardiac implantable electronic device type, manufacturer, and primary indication for placement; (3) determining whether a patient is pacing-dependent; and (4) determining the cardiac implantable electronic device’s current settings and that it is functioning properly by interrogating the cardiac implantable electronic device or obtaining the most recent interrogation report.
What is practice advisory?
Practice advisories are systematically developed reports that are intended to assist decision-making in areas of patient care. Advisories provide a synthesis of scientific literature and analysis of expert opinion, clinical feasibility data, open forum commentary, and consensus surveys. Practice advisories developed by the American Society of Anesthesiologists (ASA) are not intended as standards, guidelines, or absolute requirements, and their use cannot guarantee any specific outcome. They may be adopted, modified, or rejected according to clinical needs and constraints, and they are not intended to replace local institutional policies.
Why are practice advisories not supported by scientific literature?
They are not supported by scientific literature to the same degree as standards or guidelines because of the lack of sufficient numbers of adequately controlled studies. Practice advisories are subject to periodic revision as warranted by the evolution of medical knowledge, technology, and practice.
When to monitor electrocardiogram and Sp o2?
Continuously monitor and display a patient’s electrocardiogram and Sp o2 as required by ASA standards 66, 67 from the beginning of anesthesia until the patient is transferred out of the anesthetizing location ‡‡‡
What is the management of potential sources of electromagnetic interference associated with lithotripsy?
Management of potential sources of electromagnetic interference associated with lithotripsy consists of avoiding focus of the lithotripsy beam near the generator.