Patient Registry | Cystic Fibrosis Foundation
22 hours ago Annual Data Report 2020 Cystic Fibrosis Foundation Patient Registry 1 September 2021 Dear Friends and Colleagues: We are pleased to share the 2020 Patient Registry Annual Data … >> Go To The Portal
What is the CF Foundation patient registry?
The CF Foundation Patient Registry collects information on the health status of people with cystic fibrosis who receive care in CF Foundation-accredited care centers and agree to participate in the Registry.
Where is the CF Foundation annual data report based?
ABOUT THIS REPORT The Annual Data Report is based on data entered in the CF Foundation Patient Registry through our online portal, PortCF©. Data are entered by teams of dedicated health professionals in our nationwide network of more than 120 CF Foundation-accredited Care Centers. Inclusion Criteria
Is there a registry for cystic fibrosis?
The Cystic Fibrosis Foundation Patient Registry. Design and Methods of a National Observational Disease Registry Registries such as the CFFPR are important tools for research, clinical care, and tracking incidence, mortality and population trends.
What is the average age of someone with cystic fibrosis?
Annual Data Report 2020 Cystic Fibrosis Foundation Patient Registry 13 In 2020, the median age of people with CF in the Registry was 20.3 years. The range is from birth to 89.7 years.
See more
How do you cite the cystic fibrosis Foundation?
Cite This ItemChicago citation style: Cystic Fibrosis Foundation. Cystic Fibrosis Foundation . United States, 2002. ... APA citation style: Cystic Fibrosis Foundation. (2002) Cystic Fibrosis Foundation . United States. ... MLA citation style: Cystic Fibrosis Foundation. Cystic Fibrosis Foundation . United States, 2002.
What is CF Registry?
The CF Foundation Patient Registry collects information on the health status of people with cystic fibrosis who receive care in CF Foundation-accredited care centers and agree to participate in the Registry.
What is the epidemiology of cystic fibrosis?
There are close to 40,000 children and adults living with cystic fibrosis in the United States (and an estimated 105,000 people have been diagnosed with CF across 94 countries). Approximately 1,000 new cases of CF are diagnosed each year. More than 75 percent of people with CF are diagnosed by age 2.
How common is cystic fibrosis Worldwide?
Worldwide, about 70,000 to 100,000 people have cystic fibrosis.
How common is cystic fibrosis in Canada?
Cystic fibrosis (CF) is a rare disease affecting over 4,300 Canadians or roughly 1 in 3,600 live births. CF is a progressive, degenerative multi-system disease that affects mainly the lungs and digestive system.
Are you born with cystic fibrosis?
Cystic fibrosis (CF) is a genetic condition affecting more than 10,800 people in the UK. You are born with CF and cannot catch it later in life, but one in 25 of us carries the faulty gene that causes it, usually without knowing.
What is the main cause of cystic fibrosis?
Cystic fibrosis is caused by a change, or mutation, in a gene called CFTR (cystic fibrosis transmembrane conductance regulator). This gene controls the flow of salt and fluids in and out of your cells. If the CFTR gene doesn't work the way it should, a sticky mucus builds up in your body.
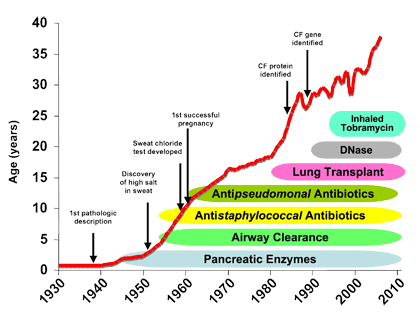
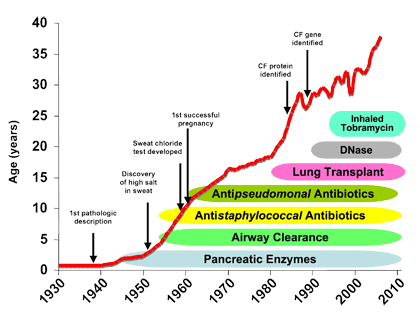
What is life expectancy of cystic fibrosis?
Outlook (Prognosis) Lung disease eventually worsens to the point where the person is disabled. Today, the average life span for people with CF who live to adulthood is about 44 years. Death is most often caused by lung complications.
What's the meaning of epidemiology?
By definition, epidemiology is the study (scientific, systematic, and data-driven) of the distribution (frequency, pattern) and determinants (causes, risk factors) of health-related states and events (not just diseases) in specified populations (neighborhood, school, city, state, country, global).
What population is most affected by cystic fibrosis?
Frequency. Cystic fibrosis is a common genetic disease within the white population in the United States. The disease occurs in 1 in 2,500 to 3,500 white newborns. Cystic fibrosis is less common in other ethnic groups, affecting about 1 in 17,000 African Americans and 1 in 31,000 Asian Americans.
Where is cystic fibrosis most common in the world?
The highest CF incidence is seen in Northern European countries with 1/3.000 live births. In the United States, the disease occurs in roughly 1 in 3.000 white Americans, 1 in 4.000-10.000 in Hispanics, and 1 in 15.000-20.000 in African Americans (10). In Africa and Asia CF is very rare.
Where is cystic fibrosis most common?
The cystic fibrosis gene is most common in Caucasians of northern European descent. The disease occurs most frequently in these people, but can occur in any ethnic population.
How many people have CF?
Background Cystic fibrosis (CF) affects >70,000 people worldwide, yet the microbiologic trigger for pulmonary exacerbations (PExs) remains unknown. The objective of this study was to identify changes in bacterial metabolic pathways associated with clinical status. Methods Respiratory samples were collected at hospital admission for PEx, end of intravenous (IV) antibiotic treatment, and follow-up from 27 hospitalized children with CF. Bacterial DNA was extracted and shotgun DNA sequencing was performed. MetaPhlAn2 and HUMAnN2 were used to evaluate bacterial taxonomic and pathway relative abundance, while DESeq2 was used to evaluate differential abundance based on clinical status. Results The mean age of study participants was 10 years; 85% received combination IV antibiotic therapy (beta-lactam plus a second agent). Long-chain fatty acid (LCFA) biosynthesis pathways were upregulated in follow-up samples compared to end of treatment: gondoate ( p = 0.012), oleate ( p = 0.048), palmitoleate ( p = 0.043), and pathways of fatty acid elongation ( p = 0.012). Achromobacter xylosoxidans and Escherichia sp. were also more prevalent in follow-up compared to PEx ( p < 0.001). Conclusions LCFAs may be associated with persistent infection of opportunistic pathogens. Future studies should more closely investigate the role of LCFA production by lung bacteria in the transition from baseline wellness to PEx in persons with CF. Impact Increased levels of LCFAs are found after IV antibiotic treatment in persons with CF. LCFAs have previously been associated with increased lung inflammation in asthma. This is the first report of LCFAs in the airway of persons with CF. This research provides support that bacterial production of LCFAs may be a contributor to inflammation in persons with CF. Future studies should evaluate LCFAs as predictors of future PExs.
What is the CFF?
The US Cystic Fibrosis Foundation (CFF) began in 1955 with a mission to support the development of new drugs to fight the disease, improve the quality of life for those with cystic fibrosis (CF), and ultimately to find a cure for this disease.1 The CFF does this by supporting basic science and clinical research in CF, supporting the care of CF patients through accredited CF centres nationwide and advocating for CF patients at the state and national level. Recognising the critical role of data collection and measurement of outcomes to better understand the natural history of CF, the CFF created a patient registry in 1966, the CFF Patient Registry (CFFPR).2 The CFFPR has evolved over the years from a few demographic variables including vital status to a comprehensive database that gives healthcare providers, researchers, policy makers and change agents data to support epidemiological and clinical research as well as efforts to improve quality of care. The specific purpose of this commentary is to describe the CFFPR and primarily to focus on how the CFFPR and its associated tools are being used for quality improvement (QI) activities, with the hope that it may help CF healthcare teams in the USA who are not familiar with the registry's capabilities, CF providers outside the USA with registries at various stages of development, and others interested in how a patient registry has been used to improve care. The CFFPR contains detailed demographic and diagnostic data dating back to 1986 with current annual and encounter-based data on over 300 unique variables including outcomes (eg, microbiology, lung function and nutritional metrics, CF complications) and care processes (eg, hospitalisations, medications, surveillance measures) for each of its more than 27 000 participants in 2012; in all, there are over 46 000 unique individuals’ data in the registry.3 …
What is PEx in CF?
Pulmonary exacerbations (PEx) in cystic fibrosis (CF) are a frequent cause of hospitalisations and lead to long-term decline in pulmonary function. Successful CF inpatient care requires the coordination of multiple providers and complex therapies. Children's Hospital of Wisconsin (CHW) and Children's Healthcare of Atlanta (CHoA) independently identified PEx inpatient care for focused improvements, with emphasis on improving care coordination and patient outcomes. Both centres began by forming multidisciplinary workgroups, including patient and family representatives. CHW's specific aim was to eliminate delays in the time to initial intravenous antibiotics. A written handoff tool was developed to allow more efficient ordering. Efforts at CHoA focused on coordination and consistent care delivery. A written schedule and patient incentive programme were devised to ensure proper administration of treatments and promote patient adherence. At CHW, interventions decreased the mean antibiotic order time by 59% with resultant decrease in administration time by 25%. At CHoA, improvements led to a 42% decrease in the proportion of hospitalisations unsuccessful in returning lung function back to within 90% of baseline. Inpatient CF PEx care is complex and requires multiple competing activities and treatments. Consistent and timely delivery of these treatments is challenging. Our improvements used the skills and insights of providers and patients to improve, standardise and synchronise care, and to develop tools to coordinate hand offs. With these improvements, applicable to hospital treatment of many other conditions, both centres were successfully able to deliver treatments in a more consistent and timely manner with improved outcomes.
What is CF in Cyprus?
Background Specialized clinical care for cystic fibrosis (CF) in Cyprus, a small island country, has been implemented since the 1990s. However, only recently, a national CF patient registry has been established for the systematic recording of patients’ data. In this study, we aim to present data on the epidemiological, genotypic and phenotypic features of CF patients in the country from the most recent data collection in 2019, with particular emphasis on notable rare or unique cases. Results Overall, data from 52 patients are presented, 5 of whom have deceased and 13 have been lost to follow-up in previous years. The mean age at diagnosis was 7.2 ± 12.3 years, and the mean age of 34 alive patients by the end of 2019 was 22.6 ± 13.2 years. Patients most commonly presented at diagnosis with acute or persistent respiratory symptoms (46.2%), failure to thrive or malnutrition (40.4%), and dehydration or electrolyte imbalance (32.7%). Sweat chloride levels were diagnostic (above 60 mmol/L) in 81.8% of examined patients. The most common identified mutation was p.Phe508del (F508del) (45.2%), followed by p.Leu346Pro (L346P) (6.7%), a mutation detected solely in individuals of Cypriot descent. The mean BMI and FEV1 z-scores were 0.2 ± 1.3 and − 2.1 ± 1.7 across all age groups, respectively, whereas chronic Pseudomonas aeruginosa colonization was noted in 26.9% of patients. The majority of patients (74.5%) were eligible to receive at least one of the available CFTR modulator therapies. In 25% of patients we recovered rare or unique genotypic profiles, including the endemic p.Leu346Pro (L346P), the rare CFTR-dup2, the co-segregated c.4200_4201delTG/c.489 + 3A > G, and the polymorphism p.Ser877Ala. Conclusions CF patient registries are particularly important in small or isolated populations, such as in Cyprus, with rare or unique disease cases. Their operation is necessary for the optimization of clinical care provided to CF patients, enabling their majority to benefit from evolving advances in precision medicine.
Does tobramycin help with CF?
Though tobramycin inhalation solution has been used for over a decade to improve lung function and reduce exacerbations in patients with cystic fibrosis ( CF), its effects on mortality have not been well-described. This study aimed to assess the association between use of tobramycin inhaled solution and mortality in patients with CF and chronic Pseudomonas aeruginosa (PA) infection. Longitudinal logistic regression was used to assess the association between current-year reported use of tobramycin inhalation solution and subsequent-year mortality of patients meeting recommended criteria for tobramycin inhalation solution use in the United States Cystic Fibrosis Foundation's Patient Registry (1996-2008). Among 12,740 patients meeting inclusion criteria, 2,538 deaths were observed during a median follow-up of 6 years. After regression adjustment, use of tobramycin inhaled solution was associated with a 21% reduction in the odds of subsequent year mortality (odds ratio (95% CI): 0.79 (0.72-0.88), P < 0.001). In our model, use of dornase alfa was also associated with a 15% reduction in the odds of subsequent year mortality (odds ratio (95% CI): 0.85 (0.76-0.95), P = 0.005). Underweight for age, CF-related diabetes, female gender, worse lung function and cultures positive for Pseudomonas aeruginosa or Burkholderia cepacia complex, among multiple other patient characteristics, were associated with significantly increased mortality. Adjusted mortality rates for patients reporting tobramycin inhalation solution use in all versus none of the follow-up years were 1.3% versus 2.1% at 2 years, 5.2% versus 8.0% at 5 years, and 9.9% versus 15.0% at 10 years. After adjustment for multiple patient characteristics and known risk factors, use of tobramycin inhalation solution was associated with significantly reduced mortality among patients with CF.