10+ Shift Report Examples in MS Word | Google Docs | PDF
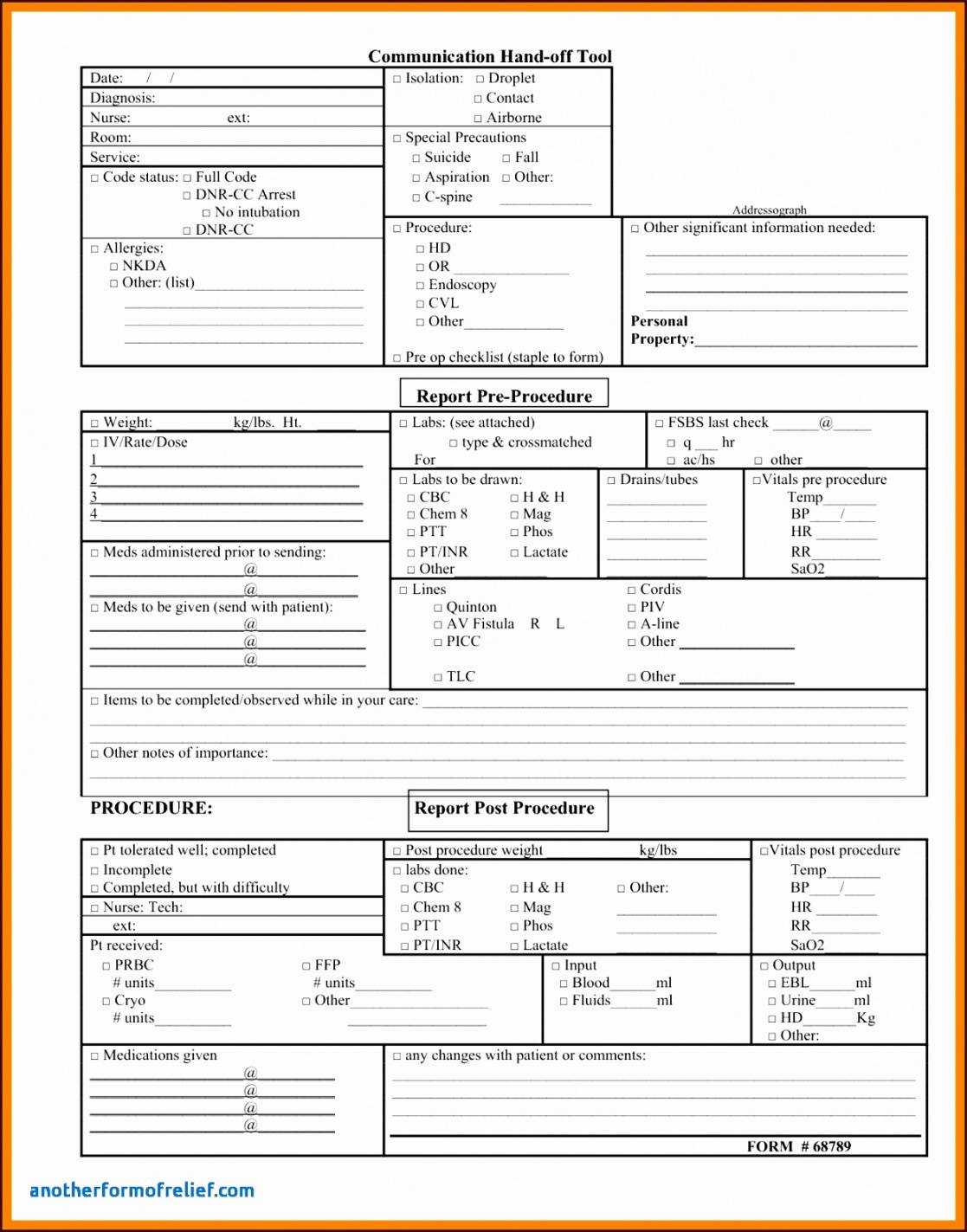
23 hours ago Below is a sample template of a shift report: End of Shift Report Template Here are some ideas for what to include in your end-of-shift report to oncoming nurses. You may also open the file of the end of shift report template here. Patient Info: Name, room, age, diagnosis, admitting physician. Assessment Information: Abnormals and pertinent ... >> Go To The Portal
What is Shift Change report in a hospital?
Having said this they work in hospitals for a stipulated time and handover their task to the nurse who takes the next shift. Therefore the communication between nurses about the patient is recorded and is called as a shift change report.
What should a nurse record in a shift report?
This section is important as the nurse must record the details monitored during their shift. The details can be the patient’s blood pressure, blood sugar, and other lab test done etc. Note: Edit this section based on your requirement and include details as desired. Next, comes the treatment details like what food is given and the future procedures.
What is the content of an employee’s shift report?
The content of an employee’s shift report may depend on what field he or she is assigned. If the employee is in the manufacturing company or anything that involves business, the shift report may contain details about the stocks.
Is there a cheat sheet for shift changes in ICU?
In ICU one may not find time to fill reports. The cheat sheet will help. We strongly recommend using the shift change report as a bedside report so that all finer details can be marked instantaneously.
How do you write a shift report?
Tips for an Effective End-of-Shift ReportUse Concise and Specific Language. ... Record Everything. ... Conduct Bedside Reporting as Often as Possible. ... Reserve Time to Answer Questions. ... Review Orders. ... Prioritize Organization. ... The PACE Format. ... Head to Toe.
What should be on a bedside shift report?
According to AHRQ, the critical elements of a BSR are: Introduce the nursing staff, patient, and family to each another. Invite the patient and (with the patient's permission) family to participate. The patient determines who is family and who can participate in the BSR.
How do you give a patient a report?
18:5620:45How to Give a Nursing Shift Report - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo you always just want to know who the family is and if you don't always look through the chart ifMoreSo you always just want to know who the family is and if you don't always look through the chart if the nurse doesn't know look through the chart. Because believe it or not to the patient.
How do you communicate with an unconscious patient?
ALWAYS talk directly to the patient during all interactions.Interact with the patient like you would anyone else.Explain what you are going to do, before you do it (examples: turning, blood draws, mouth care)Talking to the patients may reduce traumatic experiences/memories.
What is a shift report in nursing?
Background: Nurses' shift reports are routine occurrences in healthcare organisations that are viewed as crucial for patient outcomes, patient safety and continuity of care.
What is change of shift report in nursing?
Change-of-shift report is the time when responsibility and accountability for the care of a patient is transferred from one nurse to another. The communication that ensues during this process is linked to both patient safety and continuity of care giving.
How is a report written?
Reports typically stick only to the facts, although they may include some of the author's interpretation of these facts, most likely in the conclusion. Moreover, reports are heavily organized, commonly with tables of contents and copious headings and subheadings.
What is the format for report writing?
Report writing is a formal style of writing elaborately on a topic. The tone of a report and report writing format is always formal. The important section to focus on is the target audience. For example – report writing about a school event, report writing about a business case, etc.
How do you make a report?
How to write a reportDecide on terms of reference.Conduct your research.Write an outline.Write a first draft.Analyze data and record findings.Recommend a course of action.Edit and distribute.
What to do if a patient is unconscious in hospital?
What you need to doStep 1 of 5: Open the airway. Place one hand on the person's forehead and gently tilt their head back. ... Step 2 of 5: Check breathing. ... Step 3 of 5: Put them in the recovery position. ... Step 4 of 5: If you suspect spinal injury. ... Step 5 of 5: Call for help.Dealing with Someone who is Unconscious. What to do - Patient.infohttps://patient.info › signs-symptoms › dealing-with-an-ad...https://patient.info › signs-symptoms › dealing-with-an-ad...Search for: What to do if a patient is unconscious in hospital?
When a person is unconscious can they hear?
If and when the person becomes unconscious they may not be able to respond to you, however, they will still be aware of your presence and voices around them. Studies indicate that hearing is the last of the senses to be lost.Understanding the dying process - WA Healthhttps://ww2.health.wa.gov.au › Files › Corporate › Palliativehttps://ww2.health.wa.gov.au › Files › Corporate › PalliativeSearch for: When a person is unconscious can they hear?
Can patients hear when unconscious?
Twenty-five percent of all unconscious patients can hear, understand, and emotionally respond to what is happening in their external environment. However, because of their medical condition, they are incapable of moving or communicating their awareness.Perceived Unconsciousness - RnCeus.comhttp://www.rnceus.com › uncon › unperhttp://www.rnceus.com › uncon › unperSearch for: Can patients hear when unconscious?
What time do employees usually pass their reports?
Employees usually pass their reports after their shifts or during a specific time allotted by their managers.
What happens when employees pass their reports late?
Employees who pass their reports late usually get reprimanded or given a warning.
Do employees follow a certain format when making their staff reports?
Employees follow a specific format in creating staff reports. It depends on the type of format a company uses.
What to keep in mind when making an end of shift report?
When making an end-of-shift report, there are several key things nurses must keep in mind aside from just including a patient’s necessary medical information. The following are ways you can create more thorough and adequate end-of-shift reports for your relieving nurses.
What is end of shift report?
An end-of-shift report allows nurses to understand where their patients stand in regard to recovery by providing a picture of a patient’s improvement or decline over the last several hours.
What is bedside reporting?
Reviewing the end-of-shift report directly with the patient, his or her accompanying family members and the incoming nurse is often referred to by medical staff as bedside reporting. When possible, bedside reporting is typically the first thing done as a nurse arrives for a shift. This conversation provides the opportunity for all parties to ask any questions they may have before getting to work, and it also allows the patient to be actively involved in his or her own care.
Why is it important to have a detailed end of shift report?
Because understanding the personal needs of individual patients is a vital part of providing proper care, it’s important that each nurse is provided with a detailed end-of-shift report at the beginning of each new shift.
What does "Pace" mean in a report?
PACE is an acronym standing for Patient, Actions, Changes and Evaluation, all of which serve as sections in the report.
Do ICU nurses have to give special orders?
To ensure a patient receives the proper care, nurses should include special orders on each end-of-shift report and take time to review them directly with the incoming nurse.
Do nurses have to report before each shift?
Even when bedside reporting is not done before each shift, many nurses have questions regarding the end-of-shift report. It’s important to optimize the time the next nurse and the patient spend together to ensure their questions get answered and that all details of the end-of-shift report are clarified. When it comes to taking the next steps in caring for a patient, nurses are more likely to be effective when they’ve had all of their concerns addressed.
What is shift change report?
Therefore the communication between nurses about the patient is recorded and is called as a shift change report.
How to have a smooth shift change?
Reporting is the best way to have a smooth nursing shift change. Oral communication may not always help. One or two emergency cases can be reported orally to the oncoming nurse for providing immediate care. However, not all can be remembered. It is a good practice to use shift change sheet as an effective communication tool in between nurse.
What can use a patient communication sheet?
Hospitals, nursing homes, medical health care providers, and individual nurses can use this sheet for effective communication about the patient.
What does SBAR stand for in nursing?
As already stated SBAR stands for situation, background, assessment, and recommendation. Find below how a nurse can communicate their message by splitting the change report into four sections.
What is the patient identification heading?
Under the patient identification heading the patient’s name, id number given in the hospital, room number, age, gender, date of birth must be mentioned. Additional details like a patient’s father or spouse name and contact details also can be given in case if any emergency call needs to be placed by the nurse.
Why is the workload for nurses reduced?
The workload for the nurse will be reduced as they need not remember each patient’s health condition but just refer to the sheet.
What to do if you find confusion on the form?
If you find any confusion, then ask and not simply fill the form.
What is an end-of-shift report?
An end-of-shift report is a detailed report of a patient's current medical status while under your care as a nurse. When a nurse finishes their shift, they take a few minutes to record the patient's status so that the next nurse has all a patient's information when they take over their care.
Why is the end-of-shift report important?
An end-of-shift report is important because it helps the incoming nurse understand how to best care for their patients. They can quickly review a patient's medical history, allergies and the best course of action to take in case of an emergency. In addition, an end-of-shift report allows for a smooth transition from one nurse to the next.
Elements of an end-of-shift report
Different facilities include various components in their end-of-shift reports. Here are some of the typical elements found in an end-of-shift report:
How to create an end-of-shift report
Consider using this list when completing and explaining your end-of-shift report to the nurse taking over the next shift:
What is a shift report?
STANDARDIZING communication during patient handoff (shift report) is one of the 2006 National Patient Safety Goals established by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO). To meet this goal, nurses in one of our hospital's medical/surgical units decided to adopt a standardized template for handoffs between shifts. The nurse-manager asked me to investigate nursing literature and find a handoff system that would comply with JCAHO standards and unit goals.
Why do nurses keep a copy of the template?
Our nurses are encouraged to keep a copy of the template in their pocket and fill in the categories as they work. This helps them to remember important data and to give an organized and complete oral report in an efficient way.
What is intershift handoff?
Performed properly, intershift handoff lets nurses share essential information about patients with the colleagues who'll be accepting responsibility for them, ensuring continuity of care. Performed poorly, though, handoff can convey inappropriate or incomplete information and waste everyone's time.
What is the JCAHO goal?
One 2006 National Patient Safety Goal, set by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), is to “implement a standardized approach to hand off' communications.” Specifically, the JCAHO says “effective hand off' communications [should] include up-to-date information regarding the patient's/client's/resident's care, treatment and services, current condition and any recent or anticipated changes.”
What is the end of shift report for oncoming nurses?
An end of shift report is a detailed record of a patient’s current medical status. It’s written by nurses who are finishing up their shifts and are then given to nurses who are beginning their next shifts. It should include the patient’s medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
What should be included in an end of shift report?
It should include the patient’s medical history, current medication, allergies, pain levels and pain management plan, and discharge instructions. Providing these sorts of details about your patient in your end of shift report decreases the risk of an oncoming nurse putting the patient in danger.
What if you are the oncoming nurse?
If you are the oncoming nurse, the best way to receive a report is to be punctual and focused. If you are late, it shortens the window of time that the departing nurse can report on patients.
Why is it important to hand off patients?
Engaging with a patient and their families during a handoff with an oncoming nurse ensures a safe and effective transfer between shifts. It also gives nurses more time with the patients to answer questions and take care of any needs they may have.
Why don't you give every detail on a patient?
There are some areas you don’t need to give every detail on because they are either not relevant to the admitting diagnosis or something the oncoming nurse can easily look up . Using too much time on one patient will reduce the amount of time you have to give a report on the next patient.
How long does a nurse brain report take?
The amount of time you have for each patient's report depends on where you work and the nurse to patient ratio, but it's usually around 5 minutes per patient. Your Nurse's Brain can function as a nursing handoff report template. If you have kept track of this information using your Nurse’s Brain, it’s easy to quickly transfer ...
Why is handoff important in nursing?
Giving a focused, efficient report is an important communication skill in nursing. Others will respect the care and organization you put in--which can improve your nursing relationships with coworkers. Giving a good report builds trust, ensures continuity of care, and improves patient safety.
What are some examples of incident reports?
Incident reports come in several formats. Typical incident report form examples include clinical events and employee - related work injuries.
What Classifies as an ‘Incident’ That Would Prompt a Report?
In most circumstances, nurses are required to complete an incident report whenever they witness a reportable event or are notified that one has occurred. What constitutes a reportable event may vary by organization and practice setting, but the New York State Department of Health has identified some of the most common types:
What Is an Incident Report?
An incident report is an electronic or paper document that provides a detailed, written account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting. The incident doesn’t have to have caused harm to a patient, employee, or visitor, but it’s classified as an “incident” because it threatens patient safety.
How long does it take to complete an incident report?
To ensure the details are as accurate as possible, incident reports should be completed within 24 hours by whomever witnessed the incident. If the incident wasn’t observed (e.g., a patient slipped, fell, and got up on his own), then the first person who was notified should submit it.
Why are incident reports important?
Incident reports are used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for the following purposes: Risk management. Incident report data is used to identify and eliminate potential risks necessary to prevent future mistakes.
What are some examples of reportable events in New York?
Examples: adverse reactions, equipment failure or misuse, medication errors.
What information should be included in an incident report?
According to RegisteredNursing.org, the information in an incident report should always include the who, what, when, where, and how, and — at the very least — the following pertinent information:
Importance of The End-Of-Shift Report
Tips For An Effective End-Of-Shift Report
- When making an end-of-shift report, there are several key things nurses must keep in mind aside from just including a patient’s necessary medical information. The following are ways you can create more thorough and adequate end-of-shift reports for your relieving nurses.
Formatting Your End-Of-Shift Report
- With all the necessary information to include, the task of writing an end-of-shift report that’s clear and easy to read can be a challenge. Consider the following two formats to help you stay organized and communicate the right information in a concise and professional manner.
Improve Your End-Of-Shift Reports and Your Nursing Career at NDMU
- When it comes to creating proper end-of-shift reports, it’s important to put forth your best effort. Apply the same dedication to your nursing career with NDMU’s fully online RN to BSNdegree program. NDMU understands that working RNs lead busy lives, which is why this online program allows you to complete coursework on your own time, from anywhere your busy schedule takes …
What Is An End-Of-Shift Report?
- An end-of-shift report is a detailed report of a patient's current medical status while under your care as a nurse. When a nurse finishes their shift, they take a few minutes to record the patient's status so that the next nurse has all a patient's information when they take over their care. The report includes items such as the patient's name, current medications, allergies, general medica…
Why Is The End-Of-Shift Report Important?
- An end-of-shift report is important because it helps the incoming nurse understand how to best care for their patients. They can quickly review a patient's medical history, allergies and the best course of action to take in case of an emergency. In addition, an end-of-shift report allows for a smooth transition from one nurse to the next. Here are a few reasons end-of-shift reports are im…
Elements of An End-Of-Shift Report
- Different facilities include various components in their end-of-shift reports. Here are some of the typical elements found in an end-of-shift report: 1. Details of employee:It is important for the report to include employee details for record-keeping purposes. This may include your name, employee number and the department where you work. 2. Patient...
How to Create An End-Of-Shift Report
- Consider using this list when completing and explaining your end-of-shift report to the nurse taking over the next shift:
Popular Posts:
- 1. dr. dudley patient portal
- 2. u of mn vet patient portal
- 3. appletree patient portal ottawa
- 4. follow my health patient portal
- 5. first health o f the carolinas patient portal
- 6. patient portal happy healthy you
- 7. can a nurse write an incident report for withholding prn narcotics to burn patient
- 8. my mgh patient portal
- 9. marine park radiology patient portal
- 10. ascension providence waco patient portal