10+ Patient Care Report Examples [ EMS, EMT, …
35 hours ago 10+ Patient Care Report Examples 1. Partial Patient Care Report Narrative 2. Documentation of Patient Care Report >> Go To The Portal
Address the following points in a 4–6 page Patient-Centered Care Report example: Evaluate the expected outcomes of the population health improvement initiative that were, and were not, achieved. •Describe the outcomes that were achieved, their positive effects on the community’s health, and any variance across demographic groups.
Full Answer
How do you write a patient care report?
- Recognition and description of a new disease
- Recognition of rare manifestations of a known disease
- Elucidation of the mechanisms of a disease
- Detection of adverse or beneficial side effects of drugs (and other treatments)
- Medical education and audit
What are the pros and cons of patient care?
Patient-centered care is seen as a way for providers and institutions to improve patient adherence to treatment plans – and to save money by cutting wasted time. There are many positives to the model, including research showing patients who are driving their own care tend to have better outcomes, Dubbin and Shim stress.
How to write a better EMT patient care report?
- Each PCR should include all pertinent times associated with the EMS call.
- As well as the times of the assessments and treatments provided, the PCR should include detailed signs and symptoms and other assessment findings such as vital signs, and all the ...
- Also documented are changes in patient condition after treatment.
How to provide excellent patient centered care?
- The patient care environment should be peaceful and as stress free as possible. ...
- Patient safety is key. ...
- Patient care should be transparent. ...
- All caregivers should focus on what is best for the patient at all times.
- The patient should be the source of control for their care. ...

How do you write a patient care report?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
What is a patient care report used for?
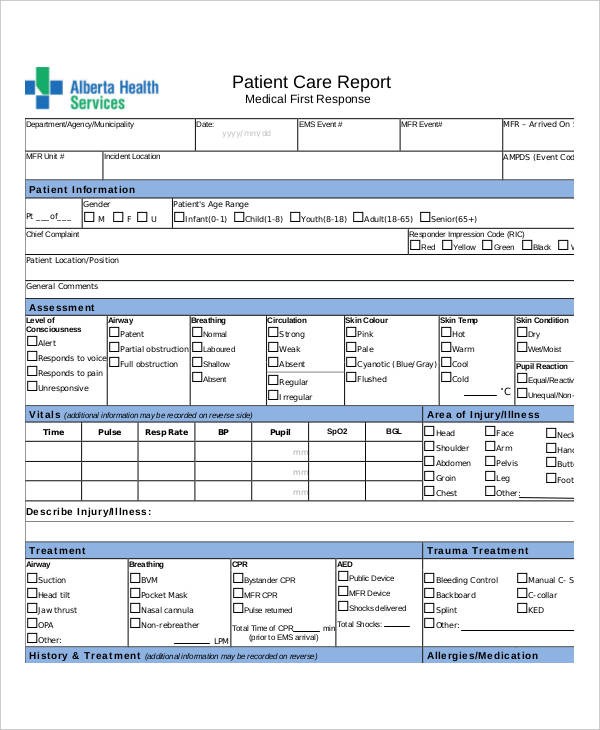
The primary purpose of the Patient Care Report (PCR) is to document all care and pertinent patient information as well as serving as a data collection tool. The documentation included on the PCR provides vital information, which is necessary for continued care at the hospital.
How do you write a proper PCR?
The following five easy tips can help you write a better PCR:Be specific. ... Paint a picture of the call. ... Do not fall into checkbox laziness. ... Complete the PCR as soon as possible after a call. ... Proofread, proofread, proofread.
What is a PCR document?
The PCR documentation is considered a medical document that becomes part of the patient's permanent medical record. It is also considered a legal document in cases where liability and/or malpractice issues arise. It is the source in which all medical billing claims are based.
What can you record on a PCR?
This includes the agency name, unit number, date, times, run or call number, crew members' names, licensure levels, and numbers. Remember -- the times that you record must match the dispatcher's times.
What is soap EMT?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What is a patient care form?
Patient care report or “PCR” means a report that documents the assessment and management of the patient by the emergency care provider.
What is an objective patient assessment finding?
Examples of objective assessment include observing a client's gait , physically feeling a lump on client's leg, listening to a client's heart, tapping on the body to elicit sounds, as well as collecting or reviewing laboratory and diagnostic tests such as blood tests, urine tests, X-ray etc.
What is pre hospital care report?
Data. The prehospital care report is used to record patient data. The data can include patient demographics such as name, address, date of birth, age, and gender. Dispatch data, such as the location of the call, times related to the call, rescuers and first responders on the scene may be included.
What is an example of PCR?
PCR allows specific target species to be identified and quantified, even when very low numbers exist. One common example is searching for pathogens or indicator species such as coliforms in water supplies.
What does PCR stand for in healthcare?
PCR (polymerase chain reaction) tests are a fast, highly accurate way to diagnose certain infectious diseases and genetic changes. The tests work by finding the DNA or RNA of a pathogen (disease-causing organism) or abnormal cells in a sample.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
Why are patient reports important?
Why Patient Reports Are Needed. Patient medical reports serve as evidences that the patient has been given proper medications or treatments. Doctors or physicians are doing the best they could in order to supply the needs of each and every patient, regardless if they are in a critical condition or not.
What is the relevant information needed for a patient complaint?
In a patient complaint, the relevant information that are needed are as follows: The description of the situation. The effect on privacy.
What is healthcare personnel?
Healthcare personnel in hospitals or medical centers ensure that they provide the needs of the patients (pertaining to the treatments or medications needed) and their individual relatives (pertaining to the answers or provision of exact details from the medical results). It goes without saying that everyone wants an accurate general information ...
What to do if you happen to be a relative of an injured person?
As the relative. If in case that you happened to be a relative of the injured person, the first thing to do is to calm down.
Do hospitals keep records of patients?
Therefore, it is mandatory that the medical clinic, center, or hospital keeps a record of their patients. These patient reports also help the doctors and the relatives of the patient to know what is or are behind the patients’ results of their individual health assessment.
Can results from medical assessments be given due to deficiency of relevant information?
Otherwise, results from medical assessments cannot be given due to deficiency of relevant information.
What questions should I ask a provider?
Here is a checklist of questions providers should answer before submitting a report: 1 Are your descriptions detailed enough? 2 Are the abbreviations you used appropriate and professional? 3 Is your report free of grammar and spelling errors? 4 Is it legible? 5 Is the chief complaint correct? 6 Is your impression specific enough? 7 Are all other details in order?
Can a report be inaccurate without proper English?
Your report should paint a picture, but this is impossible to do without proper English. Besides not being accurate or professional, incorrect English may very well lead a reader to believe something false. For example, there may be confusion (and laughter) if a report says “patient fainted and her eyes rolled around the room.” Though this is a humorous example, dire consequence can follow confusing reporting.
Why do you write PCR when you call?
Writing the PCR as soon as the call is over helps because the call is still fresh in your mind . This will help you to better describe the scene and the condition the patient was in during your call.
What should a PCR tell?
The PCR should tell a story; the reader should be able to imagine themselves on the scene of the call.
What is PCR in healthcare?
The PCR must paint a picture of what happened during a call. The PCR serves: 1 As a medical record for the patient, 2 As a legal record for the events that took place on the call, and 3 To ensure quality patient care across the service.
Why is PCR important?
A complete and accurate PCR is essential for obtaining proper reimbursement for our ambulance service, and helps pay the bills, keeps the lights on and the wheels turning. The following five easy tips can help you write a better PCR: 1. Be specific.
Why is an IV established on the patient?
This specifically explains why an IV was established on the patient and states facts that can be used to show medical necessity for the call. The same can be said for non-emergency transports between two hospitals. Simply documenting that the patient was transported for a “higher level of care” is not good enough.
How to determine if a medical necessity is met?
A primary way to determine if medical necessity requirements are met is with documentation that specifically states why you took the actions you did on a call. For example, simply documenting “per protocol” as the reason why an IV was started or the patient was placed on a cardiac monitor is not enough.
What is the purpose of PCR?
A main function of the PCR is to gather the information your service needs to bill for the call. For this to happen, the PCR needs to be detailed enough to allow the billing staff to properly code and bill for the call.
Popular Posts:
- 1. carondelet patient portal sign up stone
- 2. patient portal in sunrise features
- 3. martin's point patient portal athenahealth
- 4. "lewisbraces" patient portal
- 5. multicare patient portal
- 6. advanced obgyn patient portal huntsville al
- 7. kelsey seybold clinic patient portal
- 8. providence st mary patient portal
- 9. health quest patient portal fishkill primary care ny
- 10. nurse did not report fall and i ended up not assessing patient