Occupational Therapy, Case Study Example | essays.io
2 hours ago Rationale: Patient asks for assistance in standing up for long minutes without the need to feel extensive pain. Occupational Therapy Interventions . Preparatory Method. The client should be specifically prepared in three different aspects of development specifically considering physical, mental and emotional factors of individuality. >> Go To The Portal
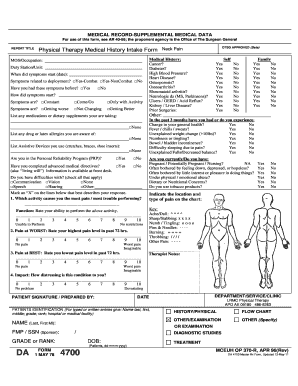
Here are two examples of a brief daily note assessment: Repeated squatting was effective in reducing pain in the patient’s low back and reinforced proper body mechanics for navigating sit to-stand transfers. This assessment statement identifies the purpose of your treatment as well as the patient’s response to your treatment.
Full Answer
What are assessments in occupational therapy?
Assessments include tools and instruments to determine occupational performance skills and measure impairments. The evaluation is a more complex process that includes interviews, observation, and use of assessments to determine impairments and measure function. Both pieces are vital parts to OT treatment.
How many assessments are there in an OT note?
We compiled over 100 assessments you can choose from to gather the most helpful data possible. The assessment section of your OT note is what justifies your involvement in this patient’s care.
What is the comprehensive occupational therapy evaluation?
The Comprehensive Occupational Therapy Evaluation (COTE) is used by OTs for patients with mental health conditions. It's a scale that identifies 25 various behavior types that are pertinent to OT practice. The COTE can be relayed to an interdisciplinary team, and it also helps to demonstrate patient progress.
Why use an occupational therapist checklist?
Information from the checklist can assist the OT in development of patient goals and the patient's plan of care. Just as evaluations vary, so do OT assessments. These diverse tools measure patient impairments and functional limitations. Again, some of them are directed at specific patient populations.
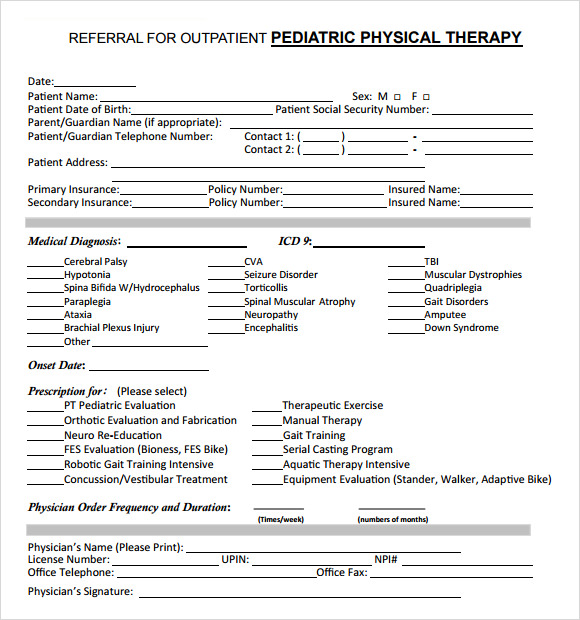
What should be included in an OT evaluation?
The OT evaluation will use assessments and tools that are appropriate based on the patient's age and individual needs. Evaluations for adolescents and young adults may include unique areas of assessment such as work, school, driving, cooking, and other activities of daily living.
How do you write a SOAP note OTA?
A SOAP note consists of the following four components:S – Subjective. This is where therapists will include information about the patient's demeanor, mood, or any changes in their medical status. ... O – Objective. ... A – Assessment. ... P – Plan. ... 4 Things To Remember With SOAP Notes.
How do you write a good occupational therapy note?
Make sure to include:Observations of how the client is performing in a specific task.How the client is performing throughout their occupational therapy session.Details about specific interventions or therapeutic activities the client engaged in and their response.
What is an assessment in occupational therapy?
An observational assessment that allows for the simultaneous evaluation of motor and process skills and their effect on the ability of an individual to perform complex or or instrumental and personal activities of daily living (ADL).
How do you write a SOAP note assessment?
SOAP Note TemplateDocument patient information such as complaint, symptoms and medical history.Take photos of identified problems in performing clinical observations.Conduct an assessment based on the patient information provided on the subjective and objective sections.Create a treatment plan.More items...•
What is SOAP note format?
The SOAP format – Subjective, Objective, Assessment, Plan – is a commonly used approach to. documenting clinical progress. The elements of a SOAP note are: • Subjective (S): Includes information provided by the member regarding his/her experience and. perceptions about symptoms, needs and progress toward goals.
How do I write an occupational therapy progress report?
The basics of an occupational therapy progress note template must include client-specific details (on each page), a review of what goals/actions were taken during the session by the client and the practitioner, and the practitioners' assessment of the client's actions, followed by corresponding updates, and ...
How can I improve my OT documentation?
Occupational Therapy Documentation: a Few GuidelinesIf You Didn't Write It Down, It Didn't Happen. ... Don't Go Overboard with Details. ... Specific Observations. ... Arguments and Hard Evidence. ... Don't Overdo Jargon. ... Be Specific About Patient Improvement. ... Note Non-Treatment Interactions Too. ... Fill in Documentation in a Timely Manner.
What kind of writing do occupational therapists do?
Four types of writing will be addressed: journal or reflective writing, developing fact sheets or handouts, technical writing specific to the profession, and scholarly writing of research papers (i.e., professional summaries, research papers, etc.).
How do you assess occupational performance?
Assessing occupational performance using the OPM(A) requires that therapists consider three primary dimensions of performance: 1) how well people are able to carry out needed and desired occupations (routines and tasks) in real world contexts where performance would typically occur, 2) identifying the person capacity / ...
What is an occupational health assessment?
An 'occupational health assessment' refers to an occupational health physician/nurse review, examination and evaluation of an individual who has been referred by their employer with regard to medical complaints and associated work absence.
What is an initial assessment in occupational therapy?
The initial assessment usually involves a discussion with you about the difficulties you may be experiencing in completing your daily occupations. These could be completing personal or domestic tasks, difficulties with mobility, accessing the community, accessing the home environment, work or education.
How do occupational therapists know what to do?
How do they know what to do in their treatment? Much of the plan of care is based on the patient's history and complaints. More data is gleaned from assessments and evaluations.
What is the Kohlman evaluation of living skills?
The Kohlman Evaluation of Living Skills (KELS) is a measure that requires patient interview and observation by the OT. Scoring is based on how much assistance a patient requires in various activities, including but not limited to self-care, money management, work, and safety.
What is the difference between an evaluation and an assessment?
The evaluation, on the other hand, is a more complex process that includes interviews, observation, and use of assessments to determine impairments and measure function.
What is Baltimore Therapeutic Equipment?
The Baltimore Therapeutic Equipment (BTE) is an electromechanical instrument that measures upper extremity strength and the ability to perform occupational tasks. This tool has adjustable resistance levels and tool handles that simulate manual work tasks. This allows OTs to assess arm strength and simulate occupational tasks.
What is a cote scale?
It's a scale that identifies 25 various behavior types that are pertinent to OT practice. The COTE can be relayed to an interdisciplinary team, and it also helps to demonstrate patient progress.
What is the NPI interest checklist?
The National Psychiatric Institute (NPI) Interest Checklist uses a self-report from the patient. This is also directed to psychiatric patients. It offers a list of 80 activities and asks the patient to rank their interest in the activity from casual to strong to no interest. There's another section that allows patients to add additional personal interests. Information from the checklist can assist the OT in development of patient goals and the patient's plan of care.
What is the Barth Time Construction tool?
The Barth Time Construction tool (BTC) requires patients to place colored papers on a chart to demonstrate how much time they spend on activities in a week, including work, self-care, and leisure activities. This is often used in patients with psychosocial dysfunction to evaluate their roles in various parts of their life.
Who approved the occupational therapy protocol?
The occupational therapy protocol was approved by the local ethical committee of Tor Vergata Policlinic and written informed consent was obtained by the patient for their participation in the study.
What is the patient's speech?
The patient’s speech is fluent and his understanding complete. He presents with good personal and social fulfillment (there are no malformations that can disturb the aesthetic appearance of the face). General conditions of the patient are good, from the diagnostic tests performed (medical visit, E.K.G., ultrasonography, spirometry) there are no alterations of the cardio-circulatory system, pulmonary or sensory apparatus. Laboratory tests are normal.
What is the assessment section of an OT note?
The assessment section of your OT note is what justifies your involvement in this patient’s care.
What should each note tell?
Each note should tell a story about your patient, and your subjective portion should set the stage. Try to open your note with feedback from the patient about what is and isn’t working about their therapy sessions and home exercise program. For example, you can say any of the following to get your note started:
What is OT potential club?
In the OT Potential Club, which is our OT evidence-based practice club, you can also access our library of documentation examples (we add one each month). They are intended to be discussion-starters to help us improve our documentation skills.
Which section of an evaluation is the longest?
The objective section of your evaluation and/or SOAP note is often the longest. This is almost certainly the case in an evaluation.
Do therapists document only one part of a story?
I think as therapists, we tend to document only one part of the story.
Do utilization reviewers hate generic language?
Not only do utilization reviewers hate that type of generic language, it robs us of the ability to demonstrate our clinical reasoning and treatment rationale!
Do OT practitioners spend time on documentation?
OT practitioners spend lots of time on documentation.
How long does occupational therapy last?
Occupational therapy services 1x/week for 30 minutes for 12 months to address the identified areas of need.
What did Robert do when he wanted the therapist's attention?
When Robert desires the therapist’s attention he stood inches from the therapist’s face and touched her mouth, demonstrating inappropriate regard for physical space in social situations. Robert exhibited intact emotional-regulation skills in situations where he was not given what he desired, however, he demonstrated disregard for authority by taking the item of desire when he thought the therapist was not watching.
Popular Posts:
- 1. my moffit patient portal
- 2. hms patient portal
- 3. crmc hospital al patient portal
- 4. unmh patient login
- 5. ambetter patient portal
- 6. hca portal access
- 7. patient portal implementation
- 8. reflections ob gyn patient portal
- 9. www.bjc.org/patient portal
- 10. do you report if patient has syphilis in florida