SOAP Report Format - Official Miami Dade College …
12 hours ago SOAP Report Guidelines for EMS Adapted from Temple College's "Key Elements of SOAP Report Format." ... 1. This is the only portion of your patient care report that should be chronological. 2. Describe what was done for the patient and how he or she responded to treatment. ... For example, if you left her purse in the tray >> Go To The Portal
How do I write a patient report in EMS?
There are seven elements (at a minimum) that we have identified as essential components to documenting a well written and complete narrative.Dispatch & Response Summary. ... Scene Summary. ... HPI/Physical Exam. ... Interventions. ... Status Change. ... Safety Summary. ... Disposition.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What is a SOAP note for EMS?
The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
How do you write a PCR narrative in EMS?
The following five easy tips can help you write a better PCR:Be specific. ... Paint a picture of the call. ... Do not fall into checkbox laziness. ... Complete the PCR as soon as possible after a call. ... Proofread, proofread, proofread.
What should be included in a SOAP note assessment?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What is objective in SOAP notes?
Objective means that it is measurable and observable. In this section, you will report anything you and the client did; scores for screenings, evaluations, and assessments; and anything you observed. The O section is for facts and data.
What is the SOAP method of charting?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
What does SOAP stand for?
Subjective, Objective, Assessment, and PlanHowever, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What should be included in a patient report?
A structured format incorporating elements of background information, medical history, physical examination, specimens obtained, treatment provided and opinion is suggested.
How do you write a patient assessment?
Assessment & PlanWrite an effective problem statement.Write out a detailed list of problems. From history, physical exam, vitals, labs, radiology, any studies or procedures done, microbiology write out a list of problems or impressions.Combine problems.
What is the soap format in a medical record?
Today, the SOAP note – an acronym for Subjective, Objective, Assessment, and Plan – is the most common method of documentation used by providers to input notes into patients' medical records. They allow providers to record and share information in a universal, systematic and easy-to-read format.
How do you write a SOAP note in nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
How do you write a SOAP note for a nurse practitioner?
9:3329:55HOW TO WRITE A SOAP NOTE / Writing Nurse Practitioner Notes ...YouTubeStart of suggested clipEnd of suggested clipSo i would write myself notes in the hpi to guide my questions that i was asking my patient. AndMoreSo i would write myself notes in the hpi to guide my questions that i was asking my patient. And then let myself know like if they say this this is what it probably means.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the inf...
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very caref...
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make...
How to fill out and sign 4-month online?
Get your online template and fill it in using progressive features. Enjoy smart fillable fields and interactivity. Follow the simple instructions below:
Accredited Business
Guarantees that a business meets BBB accreditation standards in the US and Canada.
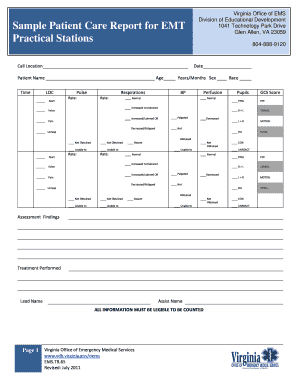
What Is a Patient Care Report?
We often hear of care reports based on by medical teams or by medical authorities. Yet, we are not sure how this differs from the kind of report that is given to us by the same people. So this is the time to make it as clear as possible.
How to Write a Patient Care Report?
Where do you even begin when you write a patient care report? A lot of EMS or EMTs do know how to write one since they are trained to do so.
What is a patient care report?
A patient care report is a document made mostly by the EMS or EMTs. This documented report is done after getting the call. This consists of the information necessary for the assessment and evaluation of a patient’s care.
What should not be written in a patient care report?
What should be avoided in a patient care report is making up the information that is not true to the patient. This is why you have to be very careful and very meticulous when writing these kinds of reports. Every detail counts.
Who is in charge of reading the patient care report?
The person or the people who will be reading the report are mostly medical authorities. When you are going to be passing this kind of report, make sure that you have all the information correctly. One wrong information can cause a lot of issues and problems.