When Must a Therapist File a Report? - Stop It Now
30 hours ago · When a patient reports a sexual relationship with a prior provider during treatment, a psychiatrist or therapist must balance conflicting ethics principles of autonomy, confidentiality, and social justice in deciding whether to report this behavior to the proper authority. Many states have statutes regarding such reporting that are unclear or ambiguous; others lack laws entirely. >> Go To The Portal
Can a psychiatrist report a sexual relationship with a patient?
Furthermore, psychiatrists are expected to report others in the profession who are “deficient in character” (Ref. 3, section 2). Thus, a psychiatrist has a clear conflict when a patient discloses a sexual relationship with a past treatment provider.
Should a prior psychotherapist's sexual exploitation of a patient be reported?
Only five states have explicit laws to address reporting of a prior psychotherapist's sexual exploitation of a patient when learned during the course of treatment (Table 2). Each state law specifically covers psychiatrists or physicians.
Are you legally obligated to report what your clients say during therapy?
However, there are some specific situations when mental health professionals are legally obligated to report something that a client does or says during a therapy session. “I like to tell my clients that therapy is kind of, ‘What happens in Vegas stays in Vegas.’
When should a therapist report a situation to protective services?
Cinéas said a therapist may have to step in and report a situation when vulnerable people are threatened, which could include children, elderly individuals and those living with a disability. “A clear case of abuse of any of the above should be reported to protective services,” she said.
What must a therapist report on a client?
What Does a Therapist Have to Tell the Police in California?Past Crimes. In most cases, discussing a past crime is protected by confidentiality rules. ... Present or Future Crimes. ... Abuse. ... Suicide.
What are the most common ethical violations in clinical psychology?
5 Major Ethical Violations In Therapycommunication of therapist's intrapsychic conflicts to the patient.contamination of the transference and consequent interpretations.the dissolution of the therapeutic “hold”the possibility of inappropriate gratification resulting from counter-transference problems.
Are therapists allowed to touch patients?
None of the professional organizations code of ethics (i.e., APA, ApA, ACA, NASW, CAMFT) view touch as unethical. Touch should be employed in therapy when it is likely to have positive therapeutic effect. Practicing risk management by rigidly avoiding touch is unethical.
Can a therapist report you?
Many states have statutes requiring healthcare providers, including mental health professionals, to report any suspected abuse of children, elders, and dependent adults. So, in most cases, therapists who hear admissions of such abuse from patients not only can report their patients' statements—they must.
What is unethical for a therapist?
Unethical behaviors by psychotherapists happen for multiple reasons. Sometimes they don't take care of themselves and find themselves using their clients to meet their personal needs. Or sometimes they might not stop and think about what they are saying and end up sharing information about a client.
What is the most common type of complaint made against professional psychologists?
found that the most common ethical issues associated with complaints against counselors were dual relationships (24%), incompetence (17%) professional misrepresentation (8%), sexual relationships with clients (7%), breach of confidentiality (5%), inappropriate fee assessments (4%), failure to obtain informed consent (1 ...
How do you deal with erotic transference?
The appropriate response to erotic transference often is to address the recent behavior in therapy without connecting it to early life experiences. This is because bringing behavior to conscious awareness without interpretation can help to minimize the risk of further “flirting” or other acting out.
Can my therapist hug me?
None of the ethics boards that regulate mental health professionals specifically prohibit the use of touch or view it as unethical. There are times when your therapist may believe that it's more harmful to you not to initiate a hug. In some cases, nonsexual, therapeutic touch may be beneficial.
Can a therapist hug their client?
Many therapists take a moderate position, offering a pat on the back or an occasional hug if the client asks for it or if a session is particularly grueling.
Are therapists obligated to report crimes?
With perhaps one exception (Under the Terrorism Act 2000 there is a requirement for certain professionals (including therapists) to disclose certain concerns relating to terrorist property), no therapist is required by law to breach confidence and inform the police that their client has committed, or is intending to ...
What are the rules of confidentiality in therapy?
Psychologists generally can't contact anyone else without your written consent. If you have specific concerns about confidentiality or what information a psychologist is legally required to disclose, discuss it with your psychologist. He or she will be happy to help you understand your rights.
Can a therapist go to jail for sleeping with a client?
Penalties for Psychologists Who Sleep with Patients But this act isn't just a civil matter and can also result in criminal charges. In most cases, the crime will be a misdemeanor punishable by up to 6 months in jail and a fine of $1000.
When a patient reports a sexual relationship with a prior provider during treatment, a psychiatrist or therapist must
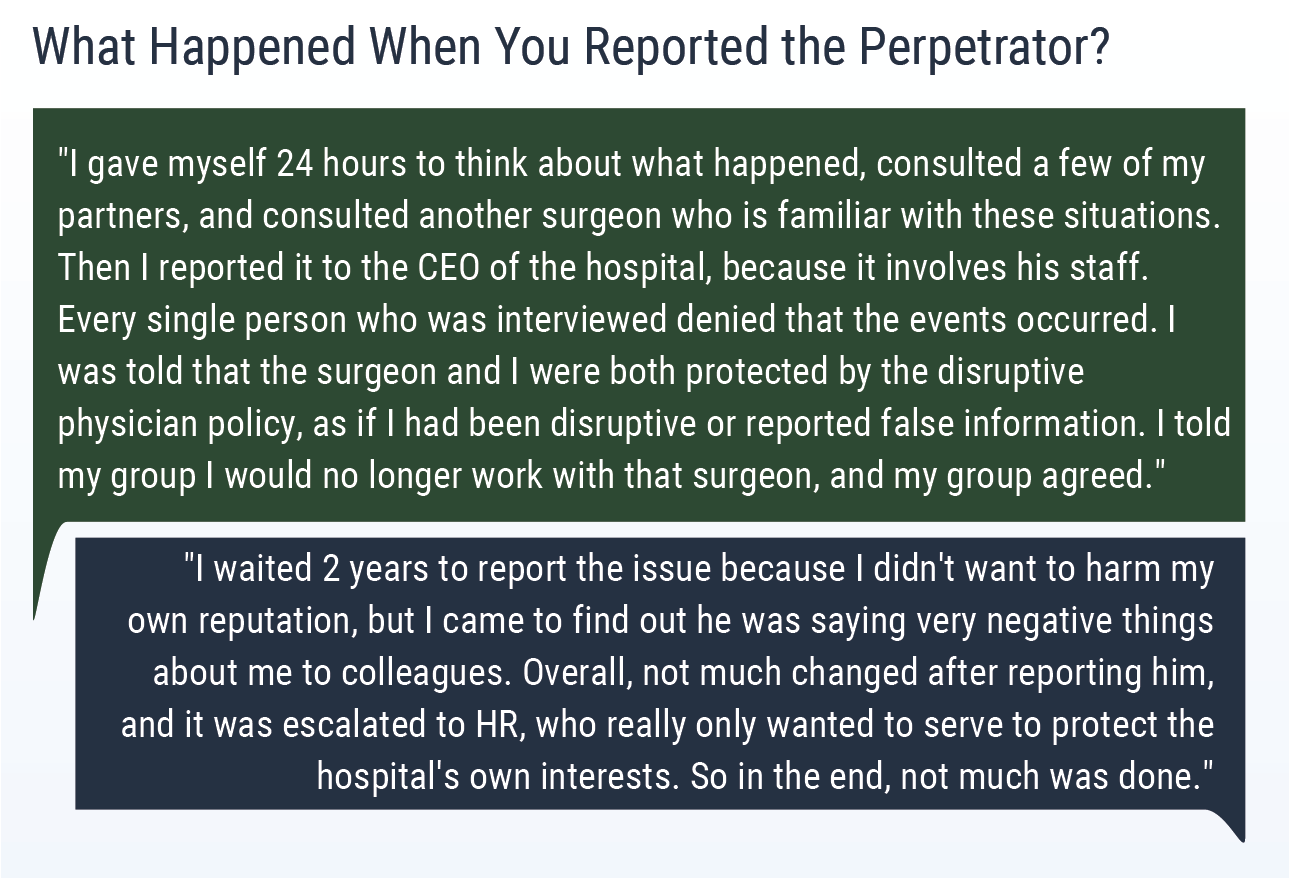
When a patient reports a sexual relationship with a prior provider during treatment, a psychiatrist or therapist must balance conflicting ethics principles of autonomy, confidentiality, and social justice in deciding whether to report this behavior to the proper authority. Many states have statutes regarding such reporting that are unclear or ambiguous; others lack laws entirely. We surveyed state laws and contacted state medical boards to clarify each state's position on mandatory reporting of sexually exploitive psychiatrists, specifically when the patient reveals the exploitation during treatment. Our results showed that only 5 state legislatures have explicitly addressed this matter. Of the remaining states, 18 require reporting through a patchwork of laws and policies, and the other 27 states and the District of Columbia have no laws that require reporting a colleague if a patient discloses a past sexual relationship. In this article, we examine the different approaches and considerations taken by state legislatures and medical boards in addressing this concern.
What percentage of psychiatrists favored mandatory reporting of therapist-patient sexual conduct?
In a survey of psychiatrists, more than one third of psychiatrists knew of a psychiatrist who had been sexually involved with patients, but only 8 percent reported the exploitation; however, 56 percent of psychiatrists favored the mandatory reporting of therapist–patient sexual conduct. 16 This discrepancy highlights the complexity of this topic. ...
What states have laws that prohibit sexual relationships between a psychotherapist and a patient?
Twenty-six states and the District of Columbia have laws that specifically forbid sexual relationships between a psychotherapist and a patient ( Table 1 ). These states use varying language to delineate the forbidden relationships. Most states specifically reference psychotherapists, mental health workers, or counselors. Alaska and Utah broadly mention health care workers, which is assumed in this article to include mental health care workers. Each of these laws, except for Colorado, provides language specifically including psychiatrists in the definition of providers banned from sexual relationships with patients.
Why are patient reports more reliable?
Laws requiring “first-hand knowledge” likely lead to more reliable reports because patient accounts can sometimes be substantially biased. They would theoretically negate the challenge of confidentiality laws because a patient report would not be first-hand knowledge of a physician's conduct.
How many states have explicit laws to address reporting of a prior sexual relationship?
Reporting Prior Sexual Relationships. Only five states have explicit laws to address reporting of a prior psychotherapist's sexual exploitation of a patient when learned during the course of treatment ( Table 2 ). Each state law specifically covers psychiatrists or physicians.
Which states have a physician's confidentiality policy?
Several states have adopted distinctive, idiosyncratic policies. Florida, 29, 30 Kansas, 31 Nebraska, 32, 33 and Nevada 34, 35 mandate physicians to report suspected unethical conduct of other physicians, but they do not allow physicians to break patient confidentiality to do so.
How many states require a physician to report a prior physician?
Reporting Rules and Laws. Thirty-three state medical boards responded with a policy, reference, or response to our inquiry. Eighteen states require a physician or psychiatrist to report a prior physician or psychiatrist for unethical conduct, even if learned from a patient in the course of confidential treatment.
What is sexual misconduct in psychiatry?
To be clear, the problem of sexual misconduct is neither limited to sexual intercourse, nor is it specific to the therapeutic environ of psychiatry. The expanded definition of physician sexual misconduct from the Federation of State Medical Boards (FSMB) includes not only grave behaviors that include sexual violation, but also misbehaviors that include sexual impropriety (i.e., behavior, gestures, or expressions that are seductive, sexually suggestive, disrespectful of patient privacy, or sexually demeaning to a patient). 9 Surveys of physicians from multiple specialties have yielded physician–patient sexual involvement rates of 3.3 to 9.8 percent, which are comparable with rates for psychiatrists. Physicians in the fields of family medicine and obstetrics and gynecology have also been disciplined at higher rates for sexual misconduct compared with their peers. 10 Additionally, a review of data from the FSMB between 1992 and 2004 indicated that 7.1 percent of all sanctions were issued for sexual misconduct irrespective of specialty. 11
Why are psychiatrists more likely to be disciplined for sexual boundary violations than their peers?
The review of literature above indicates that physician sexual misconduct continues to remain a pervasive problem and that psychiatrists are more likely to be disciplined for sexual boundary violations than their peers. Several factors could increase psychiatrists' risk of sexual boundary violations. They often work in isolation, out of view of other professionals. They have more personal contact and longer and more sessions with individual patients, hence more opportunity to become intimate with them. Patients may be more likely to report sexual misconduct for physicians of particular specialties, and psychiatric patients may be more vulnerable to inappropriate caregiver relationships. 4 The APA has recognized that psychiatrists may be more vulnerable to such violations because “the necessary intensity of the therapeutic relationship may tend to activate sexual and other needs and fantasies on the part of both patient and therapist, while weakening the objectivity necessary for control” (Ref. 15, p 4). This raises the question: Will the creation of laws mandating a duty specifically to report psychiatrists who have engaged in sexual misconduct help reduce its occurrence? MacIntyre and Appel 1 note that the rate of recidivism among psychiatrists who engage in sexual misconduct with their patients is high, and not reporting such psychiatrists can result in significant harm to subsequent patients. They note that the APA ethics guidelines allow a provider to break patient confidentiality in specific circumstances, under proper legal compulsion. 1 The authors call for special exceptions to absolute confidentiality in cases where a physician learns of sexual misconduct by a prior therapist, as with mandatory reporting policies that exist for the sexual exploitation of children and for impairment of physicians. 1
What is the primary duty of a licensing board?
Licensing boards throughout the country, in varying degrees, emphasize that their primary duty is to protect the consumer – the public – from incompetent or unprofessional licensees (those engaging in prohibited or “unprofessional conduct”) and from some who are pursuing the license. While this is a worthwhile and appropriate mission, the zeal with which protection of the public is pursued can sometimes become excessive and unfairly onerous upon those licensees that the board pursues or those applicants blocked from unfettered entry into the profession. Legislators who from time to time review the performance of licensing boards not only examine how effectively and efficiently the board processes applications for licensure, but they always concentrate on the enforcement statistics that the board presents –and licensing boards know this well.
Why is there no requirement for a subsequent therapist to report such alleged unlawful or criminal behavior on the part of
Some may ask why there is no requirement for the subsequent therapist to report such alleged unlawful or criminal behavior on the part of the prior therapist. The simple answer is that the patient’s confidentiality and privacy should be protected and should not be breached by the treating practitioner . The patient should be the one who chooses ...
Why do practitioners throw everything into a disclosure statement?
Some practitioners seem to want to throw everything into a disclosure statement in order to avoid a later claim by the patient that he or she was not made aware of something and that the failure to disclose it constituted negligence or some kind of wrongdoing or malpractice.
What is overzealous in licensing?
It is believed by some that licensing boards have been overzealous in their pursuit of applicants and licensees, including the imposition of onerous probationary terms and conditions, when the conviction of a crime is reported to the board.
Why do licensing boards need to be monitored?
Licensing board activities (e.g., supporting or opposing legislation, promulgating rules/regulations) must be monitored closely in order to protect against overreach – despite the good intentions (protecting the public) of the regulators. This California legislation (AB 2138) was passed in 2018.
When is the Avoiding Liability Bulletin?
Avoiding Liability Bulletin – March 2019. In California, when a patient reveals to a psychotherapist that during the course of a prior treatment the patient engaged in sexual intercourse or other sexual behavior or sexual conduct with the previous psychotherapist, there is a requirement to give the patient a specified brochure ...
Who was the driving force behind the Freedom of Choice Law?
Richard has been the driving force for many of the changes and additions to the laws of the State of California that affect MFTs. In 1980, he was primarily responsible for achieving passage of the "Freedom of Choice Law" that required insurance companies to pay for psychotherapy services performed by MFTs.
What happens if a therapist tells his therapist he can't stop thinking about raping
But if he told his therapist that he can’t stop thinking about raping the teenage girl next door, she is legally required to report the crime to the girl’s parents or the police. These kind of limits to therapist confidentiality in criminal cases are not limited to the informed parties either.
Who must report child abuse?
If a counselor believes an adult client has abused or neglected a child, dependent adult or elder person, the therapist must report the crime. He also must report anyone he reasonably suspected to have viewed or downloaded child pornography.
What is confidentiality in a therapist?
Therapist Confidentiality: Crimes Involving a Psychologist. Additionally, the limits to therapist/patient confidentiality mean that a mental health professional is not required to keep discussions confidential if a patient tries to use them in order to commit a crime.
Do therapists have to report crimes?
While therapists do not need to report crimes that have already happened in most cases, there are exceptions when it comes to therapist confidentiality in crimes involving crimes against children, the disabled or the elderly. This applies to both adult clients who may have committed crimes against their children or clients under 16 who have had ...
Can a psychiatrist tell if a patient has ADHD?
For example, if a patient tells her psychiatrist that she has ADHD and needs a prescription for Ritalin, but the psychiatrist can tell she is lying simply in order to obtain pills to get high, the doctor is no longer restricted by patient/doctor confidentiality laws.
Can a therapist break confidentiality?
If the patient is a minor under 16 and the therapist has reason to believe that she has been the victim of a crime and the therapist believe s it is in her best interest to report the crime, the therapist can choose to break patient confidentiality.
Do psychologists have to break confidentiality?
The most famous limits to therapist confidentiality and criminal situations is when a therapist is legally required to break confidentiality if he or she believes the patient may hurt himself or someone else. While the most obvious example of this is the mandatory institutionalization of someone who is likely to commit suicide, psychologists are also require to report patients to the police or victim if the patient indicates he or she will commit a crime against someone else.
What is the responsibility of mental health professionals to communicate the threat to the victim?
Mental health professionals must make a reasonable effort to communicate, in timely manner, the threat to the victim and notify the law enforcement agency closest to the patient's or victim's residence and supply a requesting law enforcement agency with any information concerning the threat.
When did California impose a legal duty on psychotherapists?
California courts imposed a legal duty on psychotherapists to warn third parties of patients’ threats to their safety in 1976 in Tarasoff v. The Regents of the University of California.
What is the duty of a mental health professional to protect against violent behavior?
A mental health professional has the duty to warn of or take reasonable precautions to provide protection from violent behavior only if the patient communicates an actual threat of physical violence by specific means and against a clearly identified or reasonably identifiable victim.
When can a holder of a patient's medical records disclose information?
The holder of the records may disclose information when the patient has communicated a serious threat of serious physical injury against a reasonably identifiable victim, the person with knowledge of the threat may disclose the threat to the potential victim or to any law enforcement officer, or both.
When does the duty to predict, warn, or take reasonable precautions to provide protection from, violent behavior arise?
The duty to predict, warn of, or take reasonable precautions to provide protection from, violent behavior arises only when a client or other person has communicated to the licensee a specific, serious threat of physical violence against a specific, clearly identified or identifiable potential victim.
What is client privilege in behavioral health?
Behavioral health professional - client privilege does not extend when the professional has a duty to (1) inform victims and appropriate authorities that a client's condition indicates a clear and imminent danger to the client or others; or (2) to report information required by law.
What is the Immunity for Mental Health Professionals?
Immunity for mental health professionals for release of information via 36-504 or 36-509. A release of information via 36-504 or 36-509 shall, at the request of the patient, be reviewed by a member of his family or a guardian. Section provides for appeal procedures.
What is sexual contact?
(4) "Sexual contact" means: (A) "deviate sexual intercourse" as defined by Section 21.01, Penal Code;
Who is liable for sexual exploitation?
A mental health services provider is liable to a patient or former patient of the mental health services provider for damages for sexual exploitation if the patient or former patient suffers, directly or indirectly, a physical, mental, or emotional injury caused by, resulting from, or arising out of: (1) sexual contact between the patient ...
Who is liable for damages to a mental health patient?
LIABILITY OF EMPLOYER. (a) An employer of a mental health services provider is liable to a patient or former patient of the mental health services provider for damages if the patient or former patient is injured as described by Section 81.002and the employer:
Can a mental health provider disclose a victim's identity?
The identity of an alleged victim of sexual exploitation by a mental health services provider may not be disclosed by the reporter, or by a person who has received or has access to a report or record, unless the alleged victim has consented to the disclosure in writing.
What happens if a therapist fails to take reasonable steps to protect the intended victim from harm?
“If a therapist fails to take reasonable steps to protect the intended victim from harm, he or she may be liable to the intended victim or his family if the patient acts on the threat ,” Reischer said.
Should clients withhold anything from their therapist?
“Clients should not withhold anything from their therapist, because the therapist is only obligated to report situations in which they feel that another individual, whether it be the client or someone else, is at risk,” said Sophia Reed, a nationally certified counselor and transformation coach.
Can a therapist report a patient's intent to harm someone else?
A therapist may be forced to report information disclosed by the patient if a patient reveals their intent to harm someone else. However, this is not as simple as a patient saying simply they “would like to kill someone,” according to Jessica Nicolosi, a clinical psychologist in Rockland County, New York. There has to be intent plus a specific identifiable party who may be threatened.
Do therapists have to disclose information in court?
For instance, Reed noted that even if a wife is cheating on her husband and they are going through a divorce, the therapist has no legal obligation whatsoever to disclose that information in court. The last thing a therapist wants to do is defy their patient’s trust.
Do you have to report child abuse to a therapist?
“If a client experienced child abuse but is now 18 years of age then the therapist is not required to make a child abuse report, unless the abuser is currently abusing other minors,” Mayo said.