Professional paper claim form (CMS-1500) - Centers for …
1 hours ago Dec 01, 2021 · The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of claims. It is also used for billing of some … >> Go To The Portal
Before creating a CMS-1500: Click Patients > Patient Name > Patient Billing tab Under Search Billing Transactions, click the date (s) of service you want to create a CMS-1500 for
Full Answer
How do I submit a CMS-1500 form for a client?
Dec 01, 2021 · The CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of claims. It is also used for billing of some …
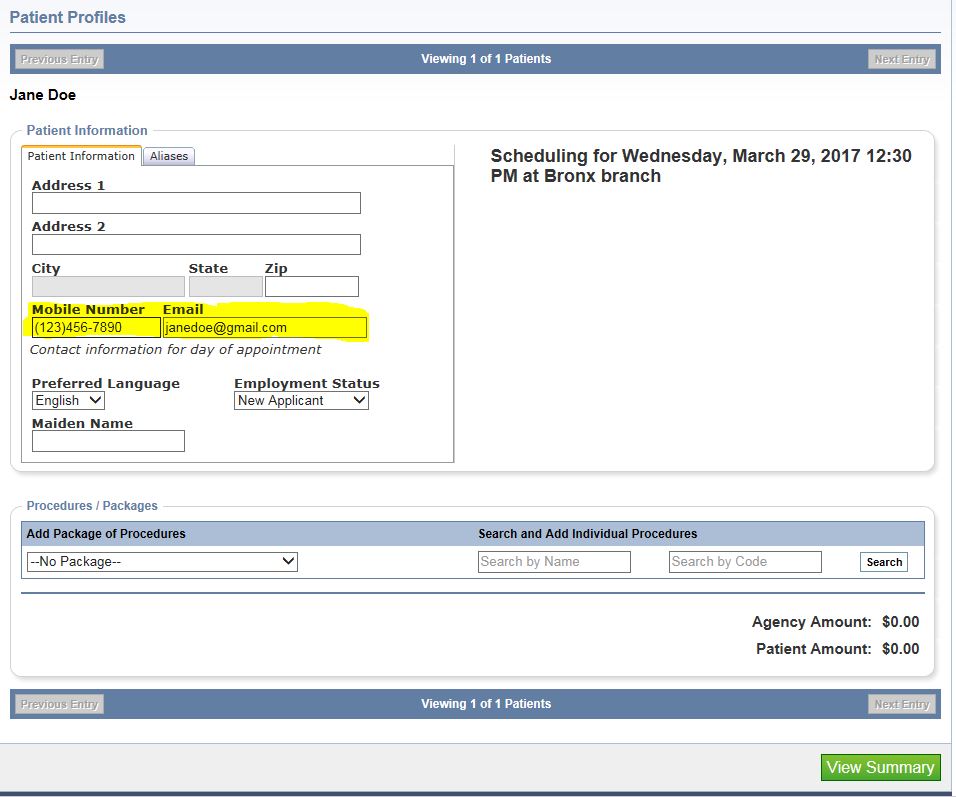
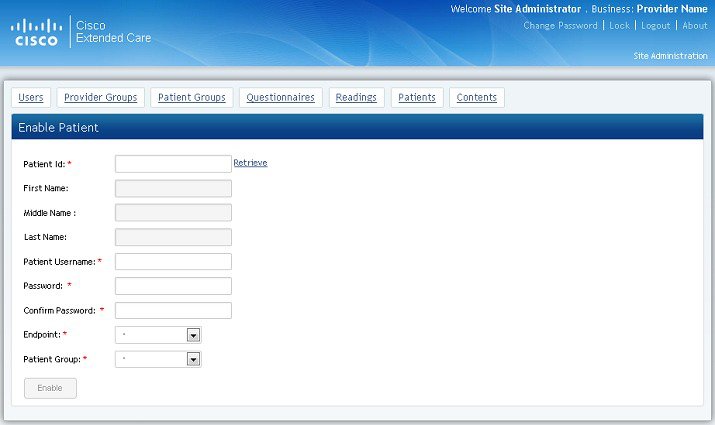
How do I sign up for the patient portal?
Dec 01, 2021 · How Electronic Claims Submission Works: The claim is electronically transmitted in data “packets” from the provider's computer modem to the Medicare contractor's modem over a telephone line. Medicare contractors perform a series of edits. The initial edits are to determine if the claims in a batch meet the basic requirements of the HIPAA ...
What is the CMS 1500 form used for?
Sep 05, 2018 · To generate a CMS-1500 form: Do one of the following. Click To-Do > Create CMS-1500 forms; Click Billing > Create CMS-1500; Click Payers > Payer Name > Payer Billing tab > Create CMS-1500; Under Search Billing Transactions, click the bold Pending Paper or Resubmit Paper link next to the date of service you want to bill for
Where can I find Medicare CMS-1500 completion and coding instructions?
patient's SFHP ID, you can log onto our provider portal to look up the patient's ID. (Insert instructions/link) 2 Required Patient's Name - Enter the member’s name as is indicated on the ID card. When submitting claims for a newborn infant using the mother’s ID number, enter the infant’s name in Box 2.
Can a provider purchase software?
Providers can purchase software from a vendor, contract with a billing service or clearinghouse that will provide software or programming support, or use HIPAA compliant free billing software that is supplied by Medicare carriers, DMEMACs and A/B MACs.
What is Medicare contractor edit?
Medicare contractors perform a series of edits. The initial edits are to determine if the claims in a batch meet the basic requirements of the HIPAA standard. If errors are detected at this level, the entire batch of claims would be rejected for correction and resubmission.
CMS-1500 Printing Options
When generating a CMS-1500 claim, TherapyNotes allows you to choose to print your data onto pre-printed red forms or print the red form background along with your data. CMS-1500 forms can be purchased from a variety of places and may be required by some payers.
Creating CMS-1500 Forms
CMS-1500 claims can be generated once a clinician completes and signs a billable note for a client who is set up to bill their insurance. The bubble next to Create CMS-1500 throughout TherapyNotes (such as on the main Billing page and on your To-Do list) will display the number of CMS-1500 claims that are ready to be submitted.
What is a CMS 1500 form?
The CMS-1500 Form is the prescribed form for claims prepared and submitted by physicians or suppliers, whether or not the claims are assigned.
When was CMS-1500 revised?
The National Uniform Claim Committee (NUCC) changed the Form CMS-1500, and the revised form received White House Office of Management and Budget (OMB) approval on June 10, 2013. The revised form is version 02/12 and has replaced the previous version of the form 08/05.
Can you include negative dollar amounts on a CMS 1500?
Negative dollar amounts are not allowed. Do not mark as continued or the claim will be rejected as unprocessable; each CMS-1500 Form should have its own total. Do not include the amount paid by the primary insurance, co-insurance, deductibles, account balance, or payments on previous claims in this item.
Do you list other supplemental coverage in item 9?
Do not list other supplemental coverage in item 9 and its subdivisions at the time a Medicare claim is filed. Other supplemental claims are forwarded automatically to the private insurer if the private insurer contracts with the carrier to send Medicare claim information electronically.
Popular Posts:
- 1. victoria mason patient message portal
- 2. dr robles el centro ca patient portal
- 3. grand traverse endo patient portal
- 4. aoaeye.com patient portal online bill
- 5. dr, maples patient portal
- 6. beatrice patient portal
- 7. campbell county health patient portal
- 8. u of m hospital ann arbor patient portal
- 9. etmc patient login
- 10. steward healthcare patient portal