Interoperability and Patient Access Fact Sheet | CMS
18 hours ago · The CMS Interoperability and Patient Access final rule establishes policies that break down barriers in the nation’s health system to enable better patient access to their health information, improve interoperability and unleash innovation, while reducing burden on … >> Go To The Portal
What is the interoperability and patient access rule (cms-9115-f)?
Overview The Interoperability and Patient Access final rule (CMS-9115-F) delivers on the Administration’s promise to put patients first, giving them access to their health information when they need it most and in a way they can best use it.
Will CMS take action against payers for payer-to-payer data exchange?
On September 15, 2021, CMS published three FAQs which explain that CMS will not take enforcement action against certain payers for the payer-to-payer data exchange provision of the May 2020 Interoperability and Patient Access final rule until future rulemaking is finalized.
How do I report eCQMs approved for CMS programs?
To report eCQMs successfully, health care providers must adhere to the requirements identified by the CMS quality program in which they intend to participate. Each year, CMS makes updates to the eCQMs approved for CMS programs to reflect changes in:
Are there any changes to the interoperability and patient access policies?
Please review the relevant FAQs for details. As of July 1, 2021, two of the policies from the May 2020 Interoperability and Patient Access final rule are now in effect. On April 30, 2021, the requirements for hospitals with certain EHR capabilities to send admission, discharge and transfer notifications to other providers went into effect.
What are the disadvantages of patient portals?
Even though they should improve communication, there are also disadvantages to patient portals....Table of ContentsGetting Patients to Opt-In.Security Concerns.User Confusion.Alienation and Health Disparities.Extra Work for the Provider.Conclusion.
How effective are patient portals?
Patient portal interventions were overall effective in improving a few psychological outcomes, medication adherence, and preventive service use. There was insufficient evidence to support the use of patient portals to improve clinical outcomes.
How does CMS impact patient care?
CMS manages quality programs that address many different areas of healthcare. These programs encourage improvement of quality through payment incentives, payment reductions, and reporting information on healthcare quality on government websites.
What impact do health care portals have on patients and patient care?
Engaging patients in the delivery of health care has the potential to improve health outcomes and patient satisfaction. Patient portals may enhance patient engagement by enabling patients to access their electronic medical records (EMRs) and facilitating secure patient-provider communication.
Why do patients not use patient portals?
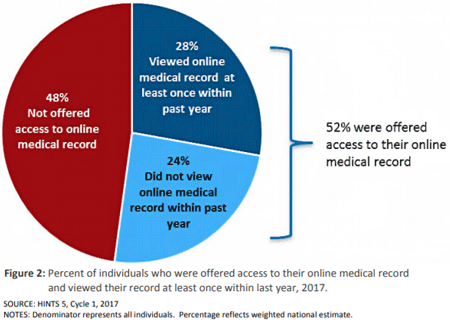
The researchers found no demographic differences among nonusers who said that a technology hurdle, lack of internet access or no online medical record was the reason why they did not make use of a patient portal.
What are the benefits and challenges of using patient portals?
What are the Top Pros and Cons of Adopting Patient Portals?Pro: Better communication with chronically ill patients.Con: Healthcare data security concerns.Pro: More complete and accurate patient information.Con: Difficult patient buy-in.Pro: Increased patient ownership of their own care.
How does CMS influence my nursing practice?
Thus, it simplifies nurses' work in that they have a solid base of medications to choose from for their patients. What concerns CMS, it helps nurses to arrange coordination within the healthcare facility, which leads to better patient outcomes (Salmond & Echevarria, 2017).
Why is the CMS important?
CMS is the organization responsible for creating health and safety guidelines for U.S. hospitals and healthcare facilities, including introducing and enforcing clinical and quality programs. As a government payor, CMS also reimburses care facilities for the healthcare services its Medicare patients receive.
What is the purpose of CMS in healthcare?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace.
What impact do health care portals have on patients and patient care quizlet?
Health care portals help patients monitor their medication usage, test results, and engage in discussions with health care providers for health care options.
When will CMS enforce interoperability and patient access?
As of July 1, 2021, two of the policies from the May 2020 Interoperability and Patient Access final rule are now in effect. On April 30, 2021, the requirements for hospitals with certain EHR capabilities to send admission, discharge and transfer notifications to other providers went into effect. On July 1, 2021, CMS began to enforce requirements for certain payers to support Patient Access and Provider Directory APIs. Additional information is available on the FAQ page and in the other information available below.
What is CMS Interoperability and Patient Access Final Rule?
In August 2020, CMS released a letter to state health officers detailing how state Medicaid agencies should implement the CMS Interoperability and Patient Access final rule in a manner consistent with existing guidance. There are many provisions in this regulation that impact Medicaid and CHIP Fee-For-Service (FFS) programs, Medicaid managed care plans, and CHIP managed care entities, and this letter discusses those issues. Additionally, this letter advises states that they should be aware of the ONC’s 21st Century Cures Act final rule on information blocking. The link for the letter is:
What is FHIR release 4.0.1?
FHIR Release 4.0.1 provides the first set of normative FHIR resources. A subset of FHIR resources is normative, and future changes on those resources marked normative will be backward compatible. These resources define the content and structure of core health data, which developers to build standardized applications.
What are IGs used for?
These guides provide information payers can use to meet the requirements of CMS rules without having to develop an independent approach, which will save time and resources. In addition, the reference implementations available on the applicable websites allow payers to see the APIs in action and support testing and development.
What is CMS 9115-F?
The Interoperability and Patient Access final rule (CMS-9115-F) put patients first by giving them access to their health information when they need it most, and in a way they can best use it. This final rule focused on driving interoperability and patient access to health information by liberating patient data using CMS authority to regulate Medicare Advantage (MA), Medicaid, Children's Health Insurance Program (CHIP), and Qualified Health Plan (QHP) issuers on the Federally-facilitated Exchanges (FFEs).
What is CMS interoperability?
When implemented effectively, health information exchange (interoperability) can also reduce the burden of certain administrative processes, such as prior authorization.
What is the payer requirement?
Payers are required to make a patient’s claims and encounter data available via the Patient Access API.
What is chronic care management?
Chronic care management services may include: Personalized assistance from a dedicated health care professional who will work with you to create a care plan. Coordination of care between your pharmacy, specialists, testing centers, hospitals, and more.
Can chronic conditions be overwhelming?
Between doctor visits, taking the right medications at the right times, and following advice from different health care professionals, managing chronic conditions like diabetes or arthritis can be overwhelming.
What is a physician value portlet?
The Physician Value Portlet allows physician and non-physician group practices and solo practitioners to view their Quality and Resource Use Reports (QRURs), and Physician Quality Reporting System (PQRS) Feedback Reports and create Value Modifier Informal Review request.
What is Enterprise Portal?
The Enterprise Portal is a gateway that provides access to over 50 different Centers for Medicare & Medicaid Services ( CMS) healthcare-based applications. It provides the ability to request access to multiple Portal-integrated CMS applications and to launch/access those applications. Learn more about Enterprise Portal.
What is DMEPOS in medical?
Durable Medical Equipment, Prosthetics, Orthotics & Supplies (DMEPOS) Bidding System - The DMEPOS Bidding System is for suppliers submitting a bid for selected products in a particular Competitive Bidding Area (CBA).
Does the HHS RoB provide guidance?
The HHS RoB cannot account for every possible situation. Therefore, where the HHS RoB does not provide explicit guidance, personnel must use their best judgment to apply the principles set forth in the standards for ethical conduct to guide their actions. [3]
What is CMS measure logic?
Measure Logic. To successfully participate in the Medicare and Medicaid Promoting Interoperability Programs, CMS requires EPs, eligible hospitals, CAHs, and dual-eligible hospitals to report on eCQMs. These eCQMs are determined by CMS and require the use of certified electronic health record technology (CEHRT).
How many ECQMs are required for EPs?
All participating EPs are required to report on any six eCQMs relevant to their scope of practice from the set of 47 available. In addition, EPs must report on at least one outcome measure. If no outcome measure is relevant to his or her scope of practice, the EP must report on one high priority measure.
Why is eCQM important?
Measuring and reporting eCQMs helps to ensure that our health care system is delivering effective, safe, efficient, patient-centered, equitable, and timely care. eCQMs measure many aspects of patient care, including: Health care providers are required to electronically report eCQMs, which use data from EHRs and/or health information technology ...

Popular Posts:
- 1. nmu health center patient portal
- 2. patient portal town and country
- 3. einstein patient portal registration
- 4. mid dakota patient portal
- 5. hampton pines emergency physicians patient portal
- 6. olympia family medicine patient portal
- 7. patient portal at shreveport internal medicine
- 8. wvu.healthcare patient portal
- 9. patient portal suzanne lamanna
- 10. pedro serrant md slidell patient portal