Recovery from dementia: An interesting case | Neurology
12 hours ago · Due to the inability to direct oneself to the various stimuli that are affecting an altered central nervous system, use of psychotropic medications may not ease the symptoms of continuous vocalizations in … >> Go To The Portal
What is the history of Neurology case reporting?
The rich history of neurology case reporting in the medical sciences traces back many generations to the time of Hippocrates (c. 460 B.C.) and, even earlier, to papyrus records of the ancient Egyptians (c. 1600 B.C.) [1, 2].
Is there a family history of dementia in first-degree patients?
There was no first-degree family history of presenile dementia. Neurocognitive assessment at the first clinic visit revealed a Mini Mental State Examination (MMSE) score of 14/30; poor verbal fluency (patient was able to produce only 5 animal names and 1 F-word in 1 min) as well as poor visuospatial and executive skills ( Fig. 1 ).
What is dementia and what are the symptoms?
Dementia is the loss of mental abilities over a period of time. People with dementia may be confused and not able to remember things. They may have difficulty especially learning new things or remembering names of people they have just met. They may get lost in places that were previously very familiar.
Can blood tests detect dementia?
A wide variety of altered levels of blood chemistry, hormones, or nutrients can cause dementia. These include altered blood count and poor kidney or liver function. Major declines in levels of thyroid hormone or vitamin B12 in the blood can also cause dementia. These are all easy to diagnose with inexpensive blood tests and can be treated.

What can a neurologist do for a dementia patient?
Neurologists are trained to detect subtleties of the brain that cause memory problems. Only they can conduct a thorough neurological exam and recommend subsequent treatment for brain disorders such as Alzheimer's.
What are the neurological symptoms of dementia?
SymptomsMemory loss, which is usually noticed by someone else.Difficulty communicating or finding words.Difficulty with visual and spatial abilities, such as getting lost while driving.Difficulty reasoning or problem-solving.Difficulty handling complex tasks.Difficulty with planning and organizing.More items...•
Is dementia related to neurology?
Visiting a primary care doctor is often the first step for people who are experiencing changes in thinking, movement, or behavior. However, neurologists — doctors who specialize in disorders of the brain and nervous system — are often consulted to diagnose dementia.
What are the neurological tests for dementia?
Mini-Mental State Examination (MMSE) This test is usually conducted by your doctor or specialist in his/her office and takes around 5 minutes to complete. The MMSE is the most common neuropsychological test for the screening of Alzheimer's disease and other causes of dementia.
What are the 7 stages of dementia?
How to Identify the 7 Stages of DementiaStage 1: No Memory Deficit.Stage 2: Slight Cognitive Decline.Stage 3: Mild Cognitive Impairment.Stage 4: Moderate Cognitive Decline.Stage 5: Moderate Dementia.Stage 6: Severe Cognitive Decline.Stage 7: Severe Dementia.
What are the 10 warning signs of dementia?
The 10 warning signs of dementiaSign 1: Memory loss that affects day-to-day abilities. ... Sign 2: Difficulty performing familiar tasks. ... Sign 3: Problems with language. ... Sign 4: Disorientation to time and place. ... Sign 5: Impaired judgement. ... Sign 6: Problems with abstract thinking. ... Sign 7: Misplacing things.More items...
Is dementia neurological or psychological?
Dementia is a psychological disorder.
What are the 4 main types of dementia?
Four Common Types of DementiaAlzheimer's Disease. This is the most common type of dementia. ... Lewy Body Dementia (or Dementia with Lewy Bodies). Lewy Body Dementia is another very common, yet frequently misdiagnosed, or undiagnosed type of dementia. ... Vascular Dementia. ... Fronto Temporal Dementia.
What are the 5 types of dementia?
There are five different types of dementia.Alzheimer's Disease. Probably the most known and the most common dementia type, Alzheimer is a consequence of an abnormal shrinkage of the brain. ... Dementia with Lewy Bodies. ... Vascular Dementia. ... Frontotemporal Dementia. ... Mixed Dementia.
What is the best test for dementia?
The Mini-Mental State Examination (MMSE)7 is the most widely applied test for dementia screening.
What is the 3 word memory test?
A third test, known as the Mini-Cog, takes 2 to 4 minutes to administer and involves asking patients to recall three words after drawing a picture of a clock. If a patient shows no difficulties recalling the words, it is inferred that he or she does not have dementia.
How is a neurological exam performed?
This may be done by using different instruments: dull needles, tuning forks, alcohol swabs, or other objects. The healthcare provider may touch the patient's legs, arms, or other parts of the body and have him or her identify the sensation (for example, hot or cold, sharp or dull). Newborn and infant reflexes.
What is a case report in neurology?
Neurology case reports have a long history of transmitting important medical information across many generations for the improvement of patient care. Case reports contribute much to the physician’s knowledge base from which treatment hypotheses and ideas form. Elements of a modern case report, as presented in the CARE (CAse REport) guidelines, include the abstract, introduction, case presentation, discussion, conclusion, patient’s perspective, and consent statement. The sections are described here, as well as the application of CARE guidelines to a published neuromuscular case report. Writing case reports offer an ideal opportunity for neurologists to publish interesting case findings and carry on the tradition of neurologic case reporting.
Who was the first person to report neurology cases?
The rich history of neurology case reporting in the medical sciences traces back many generations to the time of Hippocrates (c. 460 B.C.) and, even earlier, to papyrus records of the ancient Egyptians (c. 1600 B.C.) [1, 2]. An early description of aphasia was written by an Egyptian surgeon actually over 4000 years ago (See Fig. 1, Edwin Smith surgical papyrus, Case 20, c2800 BC) [2]. Neurology case reports throughout the centuries have contributed to our understanding of many disease entities. Hippocrates encouraged observation and was himself a keen observer. He was among the first to describe cerebrovascular disease, noting “when persons in good health are suddenly seized with pains in the head and straightaway are laid down speechless and breathe with stertor, they die in seven days when fever comes on” [3]. This author, who sees many patients with acute cerebrovascular disease, finds his characterization of subarachnoid hemorrhage apt to this day.
What are the elements of a case report?
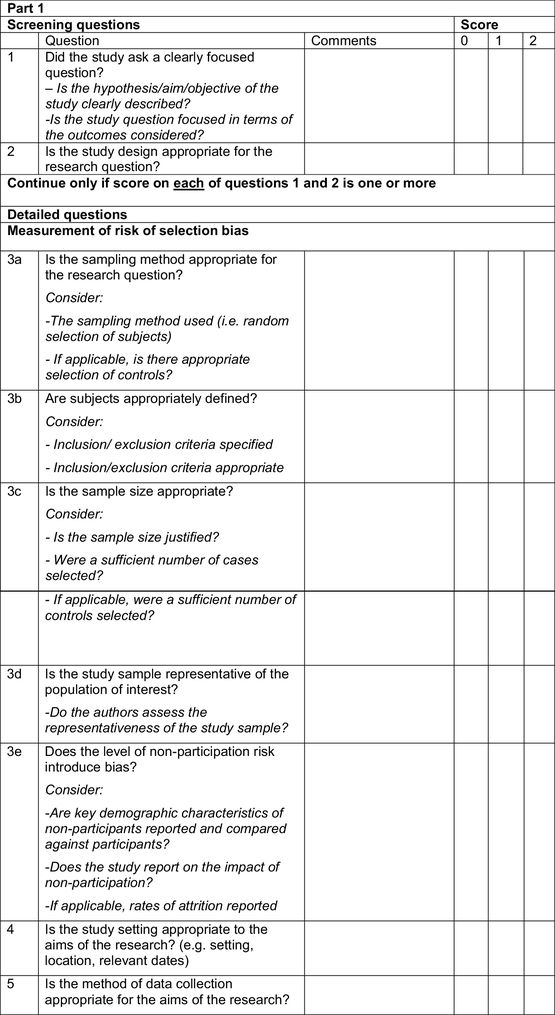
The primary items of the CARE checklist, shown in Fig. 2, are title, key words, abstract, introduction, patient information, clinical findings, timeline, diagnostic assessment, therapeutic interventions, follow-up and outcomes, discussion, patient perspective, and informed consent [15]. The CARE website describes in detail these elements and provides a summary checklist. The CARE guidelines aim to provide an international, general, non-journal-specific framework for completeness and transparency for published case reports, balancing adequate detail with concise writing [14].
What is the discussion section in JMCR?
This section compares and contrasts the case report to published literature, including a brief summary of recent literature and contemporary references. The rationale for the conclusions is given along with ways the case may be generalized to a wider population.
How to write a case report?
Much of the work that led to the decision to write a case report can be distilled in the introduction to explain the background of the case, including the disorder, usual presentation and progression , and an explanation of the presentation if it is a new disease. If it is a case discussing an adverse drug interaction, details of the drug’s common use and previously reported side effects should be detailed in the introduction. A brief literature review should give an overview of the case from the nonspecialist view. The introduction ends by stating briefly the central message of the report. A concise, salient introduction attracts a reader’s attention and serves as a sales pitch to entice the reader to continue [6].
What is case series presentation?
The presentation strikes a balance between conciseness and offering enough details for the reader to establish his or her own conclusions.
How does a case at hand present a potential contribution to medical knowledge?
Once it has been determined, through discussions and research, that the case at hand presents a potential contribution to medical knowledge, assembling the pieces of the manuscript begins.
Can BPSD be treated with nonpharmacologic therapy?
Psychotropic medications rarely address negative BPSD symptoms, while simultaneously decreasing patient's quality of life. Nonpharmacologic approaches are beneficial as first-line therapy for negative BPSD.
Is vocalization a symptom of dementia?
Vocalizations are part of the spectrum of ‘negative’ behavioral and psychological symptoms of dementia (BPSD) [1]. BPSD, also known as neuropsychiatric symptoms, constitute a major component of the dementia syndrome, regardless of the subtype. BPSD correlated strongly with the degree of functional and cognitive impairment and cause significant caregiver burden and distress [1]. It is estimated that BPSD affect up to 90% of all dementia subjects at some point during their illness, and is independently associated with poor outcomes, including distress among patients and caregivers, long-term hospitalization, misuse of medication, and increased healthcare costs [1]. As listed in table table1,1, BPSD can be divided into ‘positive’ symptoms such as agitation, aggression, hallucinations, and delusions and ‘negative’ symptoms such as passive resistance, apathy, wandering, and vocalizations.
What is the term for a neurologic emergency that can cause cerebral edema, intracranial pressure crise?
Hyperammonemia is a neurologic emergency that can cause cerebral edema, intracranial pressure crises, and seizures.
How to reduce diagnostic error?
Avoiding the trap of excessive coherence can reduce diagnostic error.
What is the purpose of identifying pathogenic gene variants in child-onset drug-resistant epilepsy?
Identification of pathogenic gene variants in child-onset drug-resistant epilepsy can be used to guide treatment in children and adults.
What is palliative care?
Palliative care aims to improve quality of life, is appropriate at any stage of illness, and can be provided alongside treatment intended to cure.
What can diagnose Wilson disease?
Clinical examination, laboratory findings, and imaging can diagnose Wilson disease .
Is cerebral edema secondary to hyponatremia?
Global cerebral edema secondary to acute hyponatremia illustrates the use of noninvasive intracranial pressure monitoring.
CASE REPORT
The patient was referred to our specialty memory clinic at the age of 58 with a 2-year history of repetitiveness, memory loss, and executive function loss. Magnetic resonance imaging scan at age 58 revealed mild generalized cortical atrophy. She is white with 2 years of postsecondary education.
DISCUSSION
β-amyloid (Aβ) is a 38 to 43 amino acid peptide that aggregates in AD forming toxic soluble oligomers and insoluble amyloid fibrils which form plaques.
Readers Of this Article Also Read
Whose Quality of Life Is It Anyway?: The Validity and Reliability of the Quality of Life-Alzheimer's Disease (QoL-AD) Scale
How old is Alice from the Neurology Department?
Alice is a 66-year-old Caucasian female, who presents to the neurology department after being referred by her primary care provider for complaints of mood swings and memory problems. Patient states, “I’ve been forgetting things. Yesterday, I couldn’t remember my dog’s name.
What is neurophysics exam?
Neurological exam: Neurophyschological exam revealed impairments on multiple cognitive tests. Many of these performances were associated with a high level of emotional distress and the patient frequently complains that she simply “couldn’t think straight.” Her behavior during the evaluation was initially well composed, she was conversant and affectively stable during the interview. During formal testing, however, she decompensated markedly and became very anxious. Her ability to tolerate frustration was minimal, and she immediately decompensated into tears with minimal cognitive challenge.