Recurrent Campylobacter jejuni bacteremia in a patient …
27 hours ago Rationale: Although some cases of recurrent bacteremia due to Campylobacter jejuni have been reported in immunocompromised patients, antibiotic treatment strategies to eradicate C. jejuni and prevent recurrent infections in immunocompromised patients have not been established. Authors' experience of such rare cases should be shared for improving patients' outcomes. >> Go To The Portal
Reported here is the case of a 78-year-old, immunocompromised male patient with Campylobacter jejuni subsp. jejuni bacteremia complicated by cellulitis. The infection was characterized by a protracted course with several recurrences and refractoriness to multiple antibiotic regimens, responding only to a prolonged course of meropenem treatment.
Full Answer
Does hypogammaglobulinemia cause recurrent Campylobacter jejuni bacteremia?
Recurrent Campylobacter jejuni bacteremia in a patient with hypogammaglobulinemia: A case report Immunocompromised patients can experience recurrent C. jejuni infection despite prolonged antibiotic therapy. Further studies to establish appropriate antibiotic therapy for eradicating colonized C. jejuni and preventing recurrent infection are needed.
What do recent outbreaks of Campylobacter suggest about epidemiologic reporting?
Recent outbreaks of campylobacter underline the importance of epidemiologic reporting and preventative measures. In 2018, there was a multi-state outbreak of Campylobacterwith a reported 113 laboratory-confirmed cases spanning over 17 states. This outbreak led to 23 hospitalizations with no reported deaths.
How common is Campylobacter infection?
Campylobacter species represent one of the most common causes of bacterial diarrheal illness worldwide. According to the United States Centers for Disease Control, there are about 1.3 million cases of Campylobacter infection each year in the United States alone.
What are the possible complications of Campylobacter infection?
There are numerous medical complications associated with Campylobacterinfection, many of which have a worse prognosis than the acute infection itself. Campylobacter infections can cause extraintestinal diseases involving the neurologic, pulmonary, immunologic and cardiac systems.
See more

How does Campylobacter affect the immune system?
For example, campylobacter production of cytolethal distending toxin both promotes an inflammatory response via IL-8 as well as assists in evasion of the immune system via arrest of the cell cycle [31]. At the same time, Toll-like receptors on intestinal epithelial cells as well as gut dendritic cells are activated.
What is the most frequently reported Campylobacter in human cases?
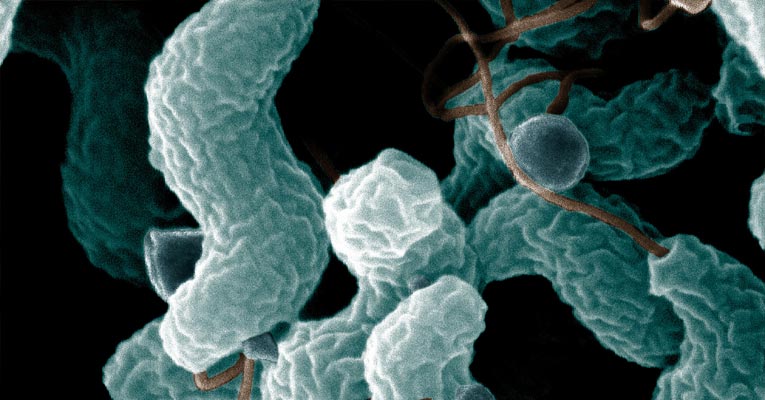
Campylobacter are mainly spiral-shaped, “S”-shaped, or curved, rod-shaped bacteria. Currently, there are 17 species and 6 subspecies assigned to the genus Campylobacter, of which the most frequently reported in human diseases are C. jejuni (subspecies jejuni) and C. coli.
Who is most susceptible to Campylobacter jejuni?
Anyone can become infected with Campylobacter but infection is more common in males, children younger than 5 years, and people 65 years and older.
What autoimmune disease is associated with Campylobacter infections?
Campylobacter infection has been associated with a number of autoimmune diseases including arthritis (particularly affecting the knee joint), Reiter's syndrome (a form of arthritis affecting the spine), conjunctivitis, and Guillain-Barré syndrome (a paralysing inflammatory disorder of the peripheral nerves).
Is Campylobacter notifiable disease?
It is caused by a bacterium known as Campylobacter. To cause illness, the bacterium must be swallowed (generally through contamination of food or water). Campylobacter is a notifiable disease.
What is the epidemiology of Campylobacter?
Anyone can get campylobacteriosis, although babies, children, and people with weakened immune systems are more likely to have serious illness. Campylobacter is one of the most common causes of diarrheal illness in the United States.
What virulence factors toxins are associated with C. jejuni pathogenesis?
C. jejuni typically colonizes the small intestine and colon through the use of virulence factors such as motility, chemotaxis, adhesion, and invasion.
What are the steps for prevention of Campylobacter jejuni?
PreventionWash Your Hands. Campylobacter and other harmful germs can survive on your hands. ... Cook Food to the Right Temperature. Be extra careful with poultry, one of the top causes of Campylobacter illnesses in the United States. ... Drink Pasteurized Milk. ... Do Not Drink Untreated Water. ... Take Care with Pets.
What are the complications of Campylobacter?
Campylobacter infections can cause extraintestinal diseases involving the neurologic, pulmonary, immunologic and cardiac systems. The main recognized sequelae are Guillain-Barré Syndrome (GBS), reactive arthritis (REA), and post-infectious irritable bowel syndrome (P-IBS).
Why does Campylobacter jejuni cause Guillain Barre?
Sometimes antibodies produced against the bacterium mimic with the host nerve gangliosides resulting in demyelination and axonal degeneration of peripheral nerves that causes Guillain-Barré syndrome.
How common is Guillain Barre after Campylobacter?
Infection with Campylobacter jejuni, which causes diarrhea, is one of the most common causes of GBS. About 1 in every 1,000 people with Campylobacter infection in the United States gets GBS.
Does Campylobacter cause inflammation?
Campylobacter bacteria, usually Campylobacter jejuni, cause inflammation of the colon (colitis) that results in fever and diarrhea. These bacteria are a common cause of infectious diarrhea in the United States and among people who travel to countries where food or water may be contaminated.
Is Campylobacter bacteremia a foodborne disease?
Campylobacter infections are most commonly associated with inflammatory diarrhea, usually due to a foodborne source. Campylobacter bacteremia is a rarely reported finding, though it has been increasingly discovered in immunocompromised patients . Though epidemiologic studies are sparse, the incidence is estimated near 0.47 per 100,000 inhabitants per year. Amongst the rarely reported cases, common underlying conditions in affected patients included liver disease, HIV infection, malignancy, solid organ transplantation, and hypogammaglobulinemia. There is a low rate of mortality associated with Campylobacter bacteremia, though the most important risk factor related to mortality is HIV infection. Further, there is no clear consensus on the optimal antimicrobial regimen for Campylobacter bacteremia, but most patients are treated given the high incidence of underlying immune compromise. About one-third of Campylobacter isolates have been shown to be resistant to fluoroquinolones, though the reported patient’s infection was susceptible to levofloxacin.
Is Campylobacter jejuni immunocompromised?
Campylobacter jejuni is an infrequent cause of bacteremia, but is most often associated with immunocompromised patients. Since there is no established guideline on the treatment of Camplyobacter bacteremia, sensitivity studies are important as they can provide insight regarding adequate antimicrobial treatment. Further, given the immunocompromised nature of many patients with Campylobacter bacteremia, prompt treatment is crucial.
Popular Posts:
- 1. gastroenterology consultants medford patient portal
- 2. archihie patient portal
- 3. heart and soul family medicine patient portal
- 4. cabrini hospital patient portal
- 5. irmc physicians patient portal
- 6. pulse md patient portal
- 7. medpeds patient portal
- 8. emory portal patient login
- 9. vsp patient portal
- 10. kidney & hypertension institute of utah patient portal