CDC - Malaria - How to Report a Case of Malaria
36 hours ago · Laboratories that have diagnosed a case of malaria should send a pre-treatment whole blood sample (EDTA) to CDC for species confirmation and evaluation for emerging drug resistance. This testing is provided free of charge and CDC will send results back to the submitter. Instructions for shipping specimens to CDC; Specimen submission form >> Go To The Portal
Test results from Malaria Rapid Diagnostic Tests are reported as either Negative or Positive. When a test result is negative, it means the individual doesn’t have any Plasmodium parasites in his/her blood. A positive result, on the other hand, means that the individual has the parasites in his/her blood and that he/she may have malaria.
How to detect malaria?
Malaria Screener: a smartphone application for automated malaria screening
- Abstract. Light microscopy is often used for malaria diagnosis in the field. ...
- Background. Microscopic examination of stained blood smears is still considered the gold standard for malaria diagnosis [ 1, 2 ].
- Implementation. ...
- Results. ...
- Discussion. ...
- Conclusions. ...
- Availability of data and materials. ...
- Abbreviations. ...
- Acknowledgments. ...
- Funding. ...
How do you test for malaria?
You’ll also get a blood test, which can tell your doctor:
- If the parasite is in your blood
- If certain medications will work against the parasite
- If your body has ever made antibodies to fight off malaria
What is the rapid diagnostic test for malaria?
- Abstract. Rapid diagnostic tests (RDTs) for malaria are a vital part of global malaria control. ...
- Background. Globally, in 2019 there were an estimated 229 million cases of malaria, including 384,000 deaths [ 1 ].
- Malaria RDT procurement and manufacturing. ...
- Analysis objective. ...
- Methods. ...
- Analysis methods. ...
- Results. ...
- Discussion. ...
- Strengths and limitations. ...
- Conclusion. ...
What is lab test for malaria?
- The results of a blood test that measures creatinine, a waste product filtered by the kidneys
- Age
- Weight
- Height
- Gender
- Race

How to identify malaria parasites?
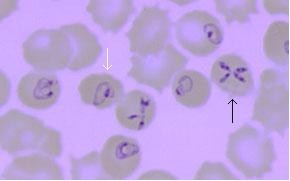
Malaria parasites can be identified by examining under the microscope a drop of the patient’s blood, spread out as a “blood smear” on a microscope slide. Prior to examination, the specimen is stained (most often with the Giemsa stain) to give the parasites a distinctive appearance.
What are the symptoms of malaria?
The first symptoms of malaria (most often fever, chills, sweats, headaches, muscle pains, nausea and vomiting) are often not specific and are also found in other diseases (such as the “flu” and common viral infections). Likewise, the physical findings are often not specific (elevated temperature, perspiration, tiredness).
Why is PCR important for malaria?
PCR is most useful for confirming the species of malarial parasite after the diagnosis has been established by either smear microscopy or RDT. More on: Molecular Diagnosis of Malaria and Babesiosis.
How long does it take to get malaria test results?
Such immunologic (“immunochromatographic”) tests most often use a dipstick or cassette format, and provide results in 2-15 minutes. These “Rapid Diagnostic Tests” (RDTs) offer a useful alternative to microscopy in situations where reliable microscopic diagnosis is not available. Malaria RDTs are currently used in some clinical settings and programs. The World Health Organization is conducting comparative performance evaluations of many of the RDTs which are commercially available worldwide based on a panel of parasites derived from a global network of collection sites. Results of this testing is available at: http://www.wpro.who.int/sites/rdt/home.htm#N#External#N#file_external#N#.
What is Molecular Characterization?
Molecular characterization: Molecular markers assessed by PCR or gene sequencing also allow the prediction, to some degree, of resistance to some drugs. CDC recommends that all cases of malaria diagnosed in the United States should be evaluated for evidence of drug resistance. More on: Drug Resistance.
Can a laboratory test show malaria?
However, for a definitive diagnosis to be made, laboratory tests must demonstrate the malaria parasites or their components. A patient with fever who had recently traveled to a malaria-endemic country is being evaluated in the emergency room. Diagnosis of malaria can be difficult:
Can a clinicist diagnose malaria?
Clinicians seeing a malaria patient may forget to consider malaria among the potential diagnose s and not order the needed diagnostic tests. Laboratorians may lack experience with malaria and fail to detect parasites when examining blood smears under the microscope.
What is malaria?
Malaria is a potentially life-threatening disease caused by the bite of infected female Anopheles mosquito which transmits the protozoa Plasmodium into your blood stream. If untreated, malaria can lead to severe morbidity, but a timely diagnosis and intervention can lead to a speedy recovery with almost no sequelae.
Why has my doctor ordered malaria antigen test for me?
Your physician may order a malaria antigen test for you if you present with the following clinical features- – High fever – Chills with rigors – Excessive sweating – Listlessness – Headache (this symptom is present in almost of the patients suffering from malaria) – Myalgia (pain in the muscles) – Arthralgia (pain in the joints) – Nausea/Vomiting – Loss of appetite – Diarrhea – Explosions of fever, associated with chills, rigors, and sweating (every 48 or 72 hours, depending on species of the malarial parasite) is a classical sign of malaria..
Can I undergo a malaria antigen test if I am pregnant?
Yes, you can safely undergo a malaria antigen test if you are pregnant or breastfeeding your child. You should keep in mind that malaria infection in a pregnant female carries a very high risk of morbidity and mortality both for the mother and the unborn child.
Can children undergo malaria antigen test?
Yes, children of all ages can undergo this test as it is a safe, risk free and easy to perform test.
Do I need to fast before a malaria antigen test?
There is no need to fast before this test. You can continue to eat and drink normally.
How should I prepare for a malaria antigen test?
No specific preparations are required before you undertake a malaria antigen test. Inform your physician if you suffer from a coagulopathy or have been taking blood thinners. Inform your physician inn detail regarding your medical history, any other drugs that you may be consuming at the time of the test and if you suffer from any drug allergy.
Are there any risks involved?
A malarial antigen test is a very safe test. It involves only a pin prick to derive blood. So, the risks involved with the technique of venipuncture are also not seen in this case. In rare cases, however, venipuncture may be resorted to.
How long does it take to get a malaria test?
The Malaria Rapid Diagnostic Tests (RDTs) can reveal the result in a span of 2 to 15 minutes.
What does the presence of a control band mean in a malaria test?
Malaria Test Results and Interpretation. Presence of “Control Band” only means test is negative. “Control” and “Test Bands” together means test is positive. And the presence of “No Control Band” means test is invalid and must be repeated test. Presence of Control Band only is considered negative.
What is the purpose of a malarial susceptibility test?
Susceptibility Testing. This test is used to detect malarial parasites which have become resistant to the drugs commonly used to treat malarial infections. There are some specialized laboratories which can test the parasites from an infected person to determine their drug susceptibility.
What is a serology test?
Serology Tests. Serology tests help in detecting antibodies in the blood that are produced by the body in response to a malaria infection. This test cannot diagnose an acute or a complicated infection but this test can certainly help in determining if the person has been previously exposed to this infection.
How does malaria affect the liver?
Once an infected Anopheles mosquito bites an individual, the plasmodium parasite then starts multiplying in the liver of the individual. In the process, the parasite starts infecting and destroying red blood cells. Malaria can be treated and controlled in case an early diagnosis can be done using specific malaria test.
What is malaria caused by?
Malaria is one mosquito borne blood disease which can often become life threatening. This disease is caused by Plasmodium Parasite and is transmitted into the human beings by a bite of a special type of mosquito – Anopheles Mosquito. Once an infected Anopheles mosquito bites an individual, the plasmodium parasite then starts multiplying in ...
What is PCR testing?
Such polymerase chain reaction is basically a laboratory method which amplifies the parasite’s DNA and allows better detection and identification of the Plasmodium species.
How to check for malaria?
What happens during a malaria test? 1 Blood smear test. In a blood smear, a drop of blood is put on a specially treated slide. A laboratory professional will examine the slide under a microscope and look for parasites. 2 Rapid diagnostic test. This test looks for proteins known as antigens, which are released by malaria parasites. It can provide faster results than a blood smear, but a blood smear is usually needed to confirm a diagnosis.
How often should you get a blood smear for malaria?
The number of malaria parasites can vary at times. So your provider may order blood smears every 12-24 hours over a period of two to three days. It's important to find out whether you have malaria so you can get treated quickly.
How long does it take for malaria symptoms to show?
But symptoms can show up as soon as seven days afterward or can take as long as a year to appear. In the early stages of infection, malaria symptoms are similar to the flu, and may include: Fever. Chills.
What is the best test for malaria?
A laboratory professional will examine the slide under a microscope and look for parasites. Rapid diagnostic test. This test looks for proteins known as antigens, which are released by malaria parasites. It can provide faster results than a blood smear, but a blood smear is usually needed to confirm a diagnosis.
What are the complications of malaria?
Left untreated, malaria can lead to life-threatening complications, including kidney failure, liver failure, and internal bleeding.
How long does it take for a blood sample to be smear?
You may feel a little sting when the needle goes in or out. This usually takes less than five minutes. Your blood sample may be tested in one or both of the following ways. Blood smear test. In a blood smear, a drop of blood is put on a specially treated slide.
How long does it take for a blood test to be done?
You may feel a little sting when the needle goes in or out. This usually takes less than five minutes.
How to check for malaria?
Other useful tests that may be done include: 1 Polymerase chain reaction (PCR). This test detects parasite nucleic acids and identifies the species of malaria parasite. 2 Complete blood count (CBC). This checks for anemia or evidence of other possible infections. Anemia sometimes develops in people with malaria, because the parasites damage red blood cells. 3 A blood glucose test. This measures the amount of a type of sugar, called glucose, in your blood.
What test is used to test for malaria?
If the doctor thinks you may have malaria, he or she will use a blood smear to check for the disease. During this test, a sample of blood is placed on a glass slide, prepared, and looked at under a microscope. A blood smear test can help diagnose malaria.
Why does malaria cause anemia?
Anemia sometimes develops in people with malaria, because the parasites damage red blood cells. A blood glucose test. This measures the amount of a type of sugar, called glucose, in your blood. Types Treatments.
What are the symptoms of malaria?
Symptoms of malaria. Symptoms may include: A very high temperature (fe ver). There may be sweats or shivering. This is a common symptom but a normal temperature does not rule out the possibility of malaria. Headaches. Tiredness. Loss of appetite.
How many people died from malaria in 2017?
It was estimated that worldwide there were 219 million cases and 435,000 deaths from malaria in 2017. The disease is uncommon in the UK. It is very rare to 'catch' malaria in the UK as the mosquitoes which transmit it cannot thrive in the UK climate.
What is the most serious parasite?
The parasite is passed to humans from a mosquito bite. There are five main types of plasmodium that cause the disease. These are called Plasmodium falciparum , Plasmodium vivax, Plasmodium ovale, Plasmodium malariae and Plasmodium knowlesi. Plasmodium falciparum is usually the most serious.
What is the cause of malaria?
Malaria is a serious infection. It is common in tropical countries such as parts of Africa, Asia and South America. It is caused by a parasite called plasmodium. A parasite is an organism that lives on an animal and feeds from it. The parasite is passed to humans from a mosquito bite.
How many cases of imported malaria in the UK?
A total of 1,792 cases of imported malaria (and six deaths from the infection) were reported in the UK in 2017. Most cases were caused by Plasmodium falciparum.
What is the most common disease that can be caught from a mosquito bite?
Malaria. Malaria is a very serious infection which you can catch from a bite from an infected mosquito. The most common symptoms are high temperature (fever) and a flu-like illness. The symptoms of malaria can occur even up to a year after travelling in an area in which malaria is present. Prompt treatment for malaria is essential, as without ...
How long does it take for a mosquito bite to show?
Symptoms usually occur between one to eight weeks after the initial mosquito bite. (This is the incubation period.) However, in some cases, depending on the type of plasmodium causing the infection, it can take up to a year before any symptoms start to show. The illness may start off with nonspecific flu-like symptoms.