Symptoms & Causes of Dengue Fever | Dengue Blood …
35 hours ago · In terms of blood investigations, leucopenia is observed usually in the course of dengue fever. Thrombocytopenia is considered a predictor of dengue hemorrhagic fever (DHF). Haemoconcentration is also a common finding due to the concentration of plasma fluid leakage, causing an increase in the haemoglobin weight in a unit volume of blood [ 17 ]. >> Go To The Portal
Interpreting a dengue blood report is not a difficult task. The reports usually contain the dengue normal value in front of the values obtained through the test. You can easily check and compare them with the normal values.The result of the whole test is found negative in the initial stage of dengue fever A mosquito borne viral disease.Dengue Fever
...
What does the test result mean?
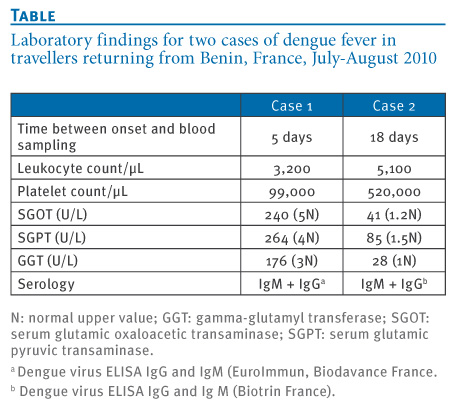
| IgM Result | IgG Result | Possible Interpretation |
|---|---|---|
| Low or negative | Positive | Past infection |
Is dengue contagious disease?
The virus is not contagious and cannot spread directly from person to person. It is mosquito-borne, so there must be a person-to-mosquito-to-another-person pathway. A mosquito bites a dengue-infected person and becomes infected with dengue. That mosquito then bites another person and passes the dengue virus infection to that person.
What causes Dengue virus?
Dengue
- Dengue Fever. Dengue is a mosquito-borne viral disease caused by the Dengue virus. ...
- Signs and Symptoms of Dengue Fever. Dengue has an unexpected attack, viz. ...
- Diagnosis of Dengue Fever. ...
- Treatment for Dengue Fever. ...
- Prevention of Dengue Fever. ...
What is the prognosis of dengue fever?
The prognosis for dengue is usually good. The worst symptoms of the illness typically last 1 to 2 weeks, and most patients will fully recover within several additional weeks. Typical dengue infection is fatal in less than 1% of cases; however, the more severe dengue hemorrhagic fever is fatal in 2.5% of cases.
How to test for dengue?
- Sudden high fever (104°F or higher)
- Swollen glands
- Rash on the face
- Severe headache and/or pain behind the eyes
- Joint and muscle pain
- Nausea and vomiting
- Fatigue
What is the normal blood count after dengue?
A typical person has a platelet count of between 150,000 and 250,000 per microlitre of blood. About 80 to 90 per cent of patients with dengue will have levels below 100,000, while 10 to 20 per cent of patients will see critically low levels of 20,000 or less.
How much platelets is normal in dengue?
Dengue fever can result in a drop in your white blood cell and platelet counts. The normal platelet count in the body ranges from 1.5 to 4 lacs, this can go down to as low as 20,000 to 40,000 in the case of dengue patients.
Can dengue be detected by CBC?
The clinical presentation of dengue patients is acute febrile illness with no localizing signs and symptoms which may mimic other infections. Therefore the laboratory tests such as a complete blood count (CBC), serological test or blood culture need to be used to differential and confirm the diagnosis.
What is the range of dengue test?
Reference Range: Dengue Fever Virus Antibody, IgG 1.64 IV or less: Negative - No significant level of detectable dengue fever virus IgG antibody. 1.65-2.84 IV: Equivocal - Questionable presence of antibodies. Repeat testing in 10-14 days may be helpful.
How do you read dengue test results?
Interpretation of resultsA positive NS1 test result confirms dengue virus infection without providing serotype information.A negative NS1 test result does not rule out infection. People with negative NS1 results should be tested for the presence of dengue IgM antibodies to determine possible recent dengue exposure.
Is 70 a low platelet count?
A platelet count below 50,000 is low. When your platelet count is low, you may bruise or bleed more easily than usual. A platelet count below 20,000 is very low.
Is CRP high in dengue?
CRP levels in patients with dengue were higher than patients with potential viral infection but lower than patients with potential bacterial infection, resulting in a quadratic association between dengue diagnosis and CRP, with levels of approximately 30 mg/L associated with the highest risk of having dengue.
What is normal WBC?
The normal number of WBCs in the blood is 4,500 to 11,000 WBCs per microliter (4.5 to 11.0 × 109/L). Normal value ranges may vary slightly among different labs. Some labs use different measurements or may test different specimens.
Why is WBC low in dengue fever?
This study may suggest that leukopenia in dengue fever may be caused by virus-induced destruction or inhibition of myeloid progenitor cells. Thrombocytopenia may result from by destruction of peripheral platelet or bone marrow megakaryocytes by viruses which consequently reduce the platelet production.
What is dengue positive report?
A positive result means you probably have been infected with the dengue virus. A negative result can mean you aren't infected or you were tested too soon for the virus to show up in testing.
How do you know dengue report is positive?
To detect the presence of the dengue virus in the blood, you need to undergo definitive tests which include non-structural protein 1 (NS1) test, Immunoglobulin G/ Immunoglobulin M test or a real time polymerase chain reaction (RT-PCR) test.
What is IgG IgM and NS1?
Dengue Antigen NS1, IgG and IgM test detects the non-structural protein component (NS1) of the dengue virus and the antibodies (IgG & IgM) produced by the body in response to the infection. NS1 and IgM is secreted into the blood during dengue infection and are detectable within 3-4 days of illness.
What are the symptoms of dengue?
Signs and symptoms of dengue may include fever, headache, rash, body aches, and bleeding manifestations. Symptoms may be mild or severe. Severe dengue often requires hospitalization. Dengue can occasionally present with signs and symptoms of aseptic meningitis or encephalitis. Dengue virus testing is not recommended for:
How long does it take to test for dengue?
Patients with symptoms consistent with dengue can be tested with both molecular and serologic diagnostic tests during the first 7 days of illness. After the first 7 days of illness, test only with serologic diagnostic tests.
How long does it take for IgM to be detected?
IgM antibodies against dengue virus can remain detectable for 3 months or longer after infection.
Can you test positive for IgM against dengue?
Therefore, a patient with other recent or past flavivirus infection (s) may be positive when tested to detect IgM antibodies against dengue virus.
Can pregnant women test for Zika?
Pregnant women: If the patient is pregnant and symptomatic and lives in or has traveled to an area with risk of Zika, test for Zika using NAAT in addition to dengue .
What test is performed for dengue?
If infection is likely to have occurred in a place where other potentially cross-reactive flaviviruses circulate, both molecular and serologic diagnostic testing for dengue and other flaviviruses should be performed.
When should you consider dengue?
Clinicians should consider dengue in a patient with a clinically compatible illness, and who lives in or recently traveled to a disease-endemic area#N#external icon#N#in the 2 weeks before symptom onset.
Can PRNTs detect IgM?
PRNTs can resolve false-positive IgM antibody results caused by non-specific reactivity, and, in some cases, can help identify the infecting virus. However, in areas with high prevalence of dengue and Zika virus neutralizing antibodies, PRNT may not confirm a significant proportion of IgM positive results.
How long does it take for dengue to be detected?
After the onset of illness, the virus can be detected in serum, plasma, circulating blood cells and other tissues for 4–5 days.
Why is dengue disease important?
early detection of severe cases, case confirmation and differential diagnosis with other infectious diseases ), surveillance activities, outbreak control, pathogenesis, academic research, vaccine development, and clinical trials.
How long does it take for an IgM antibody to appear?
IgM antibodies are the first immunoglobulin isotype to appear. These antibodies are detectable in 50% of patients by days 3-5 after onset of illness, increasing to 80% by day 5 and 99% by day 10 (Figure 4.1).
How long does it take to isolate dengue?
The isolation and identification of dengue viruses in cell cultures usually takes several days .
What are the signs of an outbreak?
During outbreaks some patients may be seen presenting with fever with or without rash during the acute illness stage; some others may present with signs of plasma leakage or shock, and others with signs of haemorrhages, while still others may be observed during the convalescent phase.
Is a diagnosis based on clinical symptoms unreliable?
Thus, a diagnosis based only on clinical symptoms is unreliable. Early laboratory confirmation of clinical diagnosis may be valuable because some patients progress over a short period from mild to severe disease and sometimes to death. Early intervention may be life-saving.