The nine rights of medication administration: an overview
28 hours ago Percent of persons using at least one prescription drug in the past 30 days: 48.6% (2015-2018) Percent of persons using three or more prescription drugs in the past 30 days: 24% (2015-2018) Percent of persons using five or more prescription drugs in the past 30 days: 12.8% (2015-2018) Source: Health, United States, 2019, table 39. pdf icon. >> Go To The Portal
What's in the annual medication access report?
In this annual report, hear from patients struggling to get the medications they need, review data on major medication access challenges and discover healthcare solutions that can make a difference. Read the full report below or download the executive summary.
Are nurses aware of the 9 rights of medications?
some nurses are not aware of the 9 Rights of Medications but it's helpful if you want to decease the errors associated with dispensing medications and improve your nursing care. I'm sharing this information because it's great for new nurses and nursing students to be aware of...
How many drugs are given or prescribed in the US?
1 Number of drugs given or prescribed: 336 million 2 Percent of visits involving drug therapy: 79.5% 3 Most frequently prescribed therapeutic classes#N#Analgesics#N#Minerals and electrolytes#N#Antiemetic or antivertigo agents 4 Analgesics 5 Minerals and electrolytes 6 Antiemetic or antivertigo agents More ...
What are the 8 right factors for right dose of drugs?
1 right patient 2 right time and frequency 3 right dose 4 right route of admission 5 right drug 6 right dilution or compatibility (important for antibiotics) 7 right flow rate (important for insulin and Heparin drips) 8 right monitoring (important for potassium, Dilantin, nitrogen drips, etc.) More items...

How many medications is considered polypharmacy?
Polypharmacy, defined as regular use of at least five medications, is common in older adults and younger at-risk populations and increases the risk of adverse medical outcomes.
Is the use of multiple medications by a patient?
The use of multiple medicines, commonly referred to as polypharmacy is common in the older population with multimorbidity, as one or more medicines may be used to treat each condition.
What are the 4 levels in a medication review?
In 'Room for Review' in 2002 they suggested four levels of medicine review – level 0 which is an ad-hoc opportunistic review; level 1 a prescription review which is a technical review of a patients list of medicines; level 2 is a treatment review which is a review of medicines with the patients full notes and level 3 ...
What percentage of elderly patients use 10 or more medications?
More than four in ten older adults take five or more prescription medications a day, tripling over the past two decades. Nearly 20 percent take ten drugs or more.
How many medications is too many?
Experts have warned for years about the dangers of taking five or more drugs at the same time — a phenomenon known as polypharmacy.
How many medications does the average adult take?
Research shows that the average older adult takes four or more prescription drugs each day, but a whopping 39 percent of seniors take five or more prescriptions each day. While each one was created to treat or manage a specific medical problem, each also comes with its own risks and side effects.
What is a Level 1 medication review?
Types of Review Description Type 1 Prescription review: addresses issues relating to the prescription or medicines; the patient does not need to be present, nor access to full notes.
What is treatment chart review?
Treatment Chart Review is a process where a pharmacist reviews the patient's drug treatment during his hospital admission and involves evaluation of the therapeutic efficacy of each drug and the progress of the conditions being treated.
How do you do a medication review?
What happens at a medicines review? You will be asked to make an appointment with your doctor, pharmacist or nurse for a medicines review. The review will take between 10 and 30 minutes. The review will involve the doctor/pharmacist/nurse gathering information from you and from your medical record.
What is the average number of prescriptions per person?
How many prescriptions does the average American take? Data suggests that among those who take prescription medications, the average number of medications taken is four. More than 131 million Americans take at least one prescription medication.
What percentage of adults take 5 or more medications?
More than 40 percent of older Americans regularly take five or more prescription drugs, and nearly 20 percent take 10 or more, according to a 2020 report from the nonpartisan think tank Lown Institute.
What percentage of older adults take 5 or more medications?
Among U.S. adults aged 40–79, 69.0% used one or more prescription drugs in the past 30 days and 22.4% used five or more (Figure 1).
What is multiple prescribing?
Polypharmacy is defined as the use of multiple medications by a patient, with 5–10 medications usually accepted as the cutoff. From: Geriatric Rehabilitation, 2018.
What happens when you take too many medications?
The more medications you are taking, the higher the risk of those drugs interacting dangerously with each other. Multiple medications can cause confusion, lightheadedness and even internal bleeding — all dangerous and injurious conditions.
What does it mean to take medications together?
An interaction is when one medicine affects how another medicine works. For example, taken together, one medicine may make the other medicine stronger. Medicines can also interact with alcohol and even some foods. Some interactions can be serious, even life threatening.
Can you take multiple medicines at the same time?
As long as a doctor or pharmacist has taken into account the effect of taking two or more medicines at the same time it should be perfectly safe.
What are the nine rights of medication administration?
The nine rights of medication administration: an overview. Nurses are responsible for ensuring safety and quality of patient care at all times. Many nursing tasks involve a degree of risk, and medication administration arguably carries the greatest risk. Unfortunately, patients are frequently harmed or injured by medication errors.
How many rights do nurses have?
Some suffer permanent disability and for others the errors are fatal. Nurses have traditionally followed the five rights of medication administration (patient, drug, route, time, dose) to help prevent errors, and more recently, the seven rights (including documentation and reason).
Do nurses have to be harmed by medication errors?
Unfortunately, patients are frequently harmed or injured by medication errors. Some suffer permanent dis …. Nurses are responsible for ensuring safety and quality of patient care at all times. Many nursing tasks involve a degree of risk, and medication administration arguably carries the greatest risk. Unfortunately, patients are frequently harmed ...
What are the rights of a nurse?
some nurses are not aware of the 9 Rights of Medications but it's helpful if you want to decease the errors associated with dispensing medications and improve your nursing care. I'm sharing this information because it's great for new nurses and nursing students to be aware of... Furthermore, every medication given should at least follow the first 5 rights but some medications are very important in other areas so more rights were added: 1 right patient 2 right time and frequency 3 right dose 4 right route of admission 5 right drug 6 right dilution or compatibility (important for antibiotics) 7 right flow rate (important for insulin and Heparin drips) 8 right monitoring (important for potassium, Dilantin, nitrogen drips, etc.) 9 right documentation (very important for tPa, conscious sedation) and the right documentation usually includes forms to help or know the "right monitoring"
Do you need 10 or 15 rights?
You do not need 10 or 15 rights! This is why errors happen, cos students/nurses are trying to learn and integrate too many things at once. Keep it simple with the 5 rights - you don't need how to dilete, right site, etc, etc. That's just pedantics. You are trained to read the order and your drug book.
Should a nurse say OK to a patient's refusal?
Of course, the nurse shouldn't just say "OK" to the patient's refusal and leave it at that. It's up to the nurse to educate the patient, make sure he understands the consequences of not taking the medicaiton...and if he still refuses to document the education and the refusal.
Do nurses have rights to medication?
some nurses are not aware of the 9 Rights of Medications but it's helpful if you want to decease the errors associated with dispensing medications and improve your nursing care. I'm sharing this information because it's great for new nurses and nursing students to be aware of... Furthermore, every medication given should at least follow ...
Is monitoring and assessing a nursing practice?
Monitoring and assessing is standard nursing practice and doesn't need to be included in this list. If monitoring was on this list than we might as well add, right notification to the MD, right lab draws afterward, right follow up assessment, right report to the oncoming shift. i mean really....?
Is it good to have 9 rights?
The 9 rights are good...but IMO it should be 10. You're missing the right to refuse a medication, both on the part of the nurse and the patient. Unless under court order, a patient has the legal right to refuse any medication even if doing so would be detrimental to his health.
How many prescriptions are there for levothyroxine?
Levothyroxine: 101.9 Million Prescriptions. The third on the list of the most used drugs in the U.S. is this hypothyroidism treatment, sold under brand names like Levo-T, Synthroid, Euthyrox, and Levoxyl.
How many people are affected by hypothyroidism?
Hypothyroidism affects 4.6% of the population ages 12 and up and can lead to a host of issues, from weight gain to depression. 4. Metformin: 78.6 Million Prescriptions. More than 100 million patients in the U.S. are living with diabetes or pre-diabetes, according to the CDC.
How much does a left ventricular hypertrophy prescription cost?
This prescription is a bit more expensive, though, at an average of $128.90.
How much does Amlodipine cost?
5. Amlodipine: 72.5 Million Prescriptions. Another one of the commonly prescribed medications for high blood pressure, chest pain, and coronary artery disease, this drug is a bit cheaper than alternatives, with an average cost of $27.34. Brand-name versions like Norvasc, Katerzia, and Amvaz may be more expensive, however.
How much does rosuvastatin cost?
For example, rosuvastatin, a cholesterol medication, averages an absurd retail price of $433.82. Meanwhile, the humble aspirin, one of the most common drugs available, only costs an average of $3.86.
What is the most prescribed ACE inhibitor?
1. Lisinopril: 104 Million Prescriptions. Selling under brand names like Prinivil and Zestril, this ACE inhibitor is the most prescribed medication in the United States. It’s used for high blood pressure treatment and heart failure prevention to help improve survival after a heart attack.
Which is more expensive, Norvasc or Metoprolol?
Brand-name versions like Norvasc, Katerzia, and Amvaz may be more expensive, however. 6. Metoprolol: 68 Million Prescriptions. Heart attacks are extremely common, and prescribed drugs like Lopresso and Toprol provide treatment for high blood pressure and chest pain as a treatment for heart failure.
How long does it take for a medication to be given?
Medications generally need to be given within 30 minutes of the prescribed time to be given. If a medication is to be given at 10 a.m. then you may give it any time between 9:30 a.m. and 10:30 a.m. Some medications may need to be given specifically before or after lunch and this time may vary by grade level. Any time outside of this time frame would not be the right time to give the medication. Many medications need to sustain a “drug level” in the blood stream to be effective. Therefore not giving them at a certain time can affect the way the medication is intended to work. This is especially important with medications for Attention Deficit Disorders and Seizures and some antibiotics. If a student receives medication in the early morning at school and arrives late to school, check with the parent to verify if the student has taken the medication prior to coming to school. Also, for medications given later in the afternoon, remind parents that on early release days the medication will not be given at school that day.
What are the routes of medication?
Routes of medications include oral, topical, instilled in eyes or ears and inhaled. Oral medications are taken by mouth and include tablets, capsules, elixirs and suspensions. Topical medications are applied to the skin and include medicated ointments and creams, medicated eye, ear and /or nose drops. Inhaled medications are suspended in an aerosol and inhaled into the lungs and include inhalers and nebulizer treatments. The majority of medications given at school will be given orally.
When do you have to pick up medication at school?
When medications must be taken at school it is the parent/guardian’s responsibility to supply the school with the medication and to pick up any unused medication either at the end of the school year or when the student’s healthcare provider discontinues the medication.
What are the primary subcategories of medications?
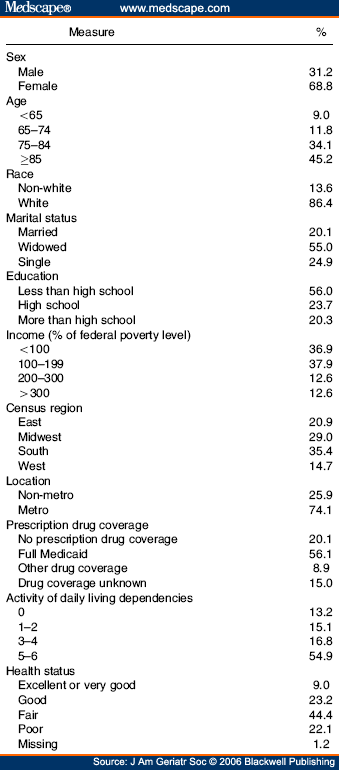
Primary medication subcategories of interest included statins, antihypertensives, antidiabetic agents, antidepressants, and PIMs. Ingredient-level coding from Lexicon Plus was used to identify medications containing therapeutic drug classes of interest. Generic medication names were used to identify PIMs. PIM use was defined based on the 2003 Beers List (8), which was the most recent criteria relevant to the NHANES cycles of interest; it was applied to all years to reveal meaningful changes in PIM use that were not simply a by-product of changing guidelines. The Beers List makes some recommendations specific to diagnosis, condition, dose, and duration; medications specific to these recommendations were not included. The list used in the present study is summarized in Supplementary Table S1.
When did prescription medication use increase?
Prescription medication use increased dramatically among older adults between 1988 and 2010. Contemporary older adults on multiple medications have worse health status compared with those on less medications, and appear to be a vulnerable population.
What is polypharmacy in older adults?
Older adults have a high prevalence of multiple chronic health conditions for which multiple medications are typically recommended as treatment (1,2). Consequently multiple medication use, often referred to as polypharmacy, is common in this population (1). Polypharmacy may be problematic for a number of reasons. For example it may increase the risk of using potentially inappropriate medications (PIMs) (3,4), which have been associated with negative effects on long-term physical and cognitive functioning (5). Polypharmacy also results in medication nonadherence (1,6), increased risk of drug duplication, drug–drug interactions (1) and adverse drug reactions (ADRs) (1,6,7), and higher health care costs (6,8,9). Research has also found that medication use may be associated with poor functional status (6), and decreased cognitive capacity (10). Given the rapidly aging population and the potential negative effects of multiple medication use, it is of interest to characterize trends and correlates of polypharmacy in older adults.
Why is medication use increasing?
Rising medication use likely represents increasing awareness and treatment of disease, as well as improved access and availability of drug therapies. This may be largely beneficial; however, prescription medication use is not without risks. Side effects such as reduced alertness, vision, and muscle strength may occur, possibly leading to decreased physical functioning (28). Increased medication use also increases risk of ADRs, and ADRs resulting in hospitalization may lead to other adverse outcomes for older adults (7). In our study, we observed that participants taking more medications were more likely to have a functional limitation, ADL limitation, or confusion/memory problems. This is concerning because older adults with decreased physical and cognitive ability may be more susceptible to the unintended consequences of prescription medication use, including side effects, ADRs, and associated sequelae. Increased susceptibility to side effects and ADRs may also increase the likelihood of prescribing cascades, whereby drug-related symptoms are misdiagnosed as new health problems, and additional drugs are prescribed to address them (2). Such processes increase medication burden in an already vulnerable population.
Do older adults need multiple medications?
Older adults frequently have several chronic health conditions which require multiple medications. We illustrated trends in prescription medication use over 20 years in the United States, and described characteristics of older adults using multiple medications in 2009–2010.
Who published The Author 2015?
Copyright© The Author 2015. Published by Oxford University Press on behalf of The Gerontological Society of America. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com.
Is polypharmacy a public health concern?
population continues to age, polypharmacy will become an increasingly crucial issue. Considering the risks of polypharmacy, rising prescription medication use is an important public health concern that warrants the attention of clinicians, policymakers, and further research. Many approaches to medication management have been investigated, including clinical decision support systems to guide evidence-based prescribing and involvement of clinical pharmacists in collaborative care. Implementation of methods to manage polypharmacy among the community-dwelling elderly will be critical to the delivery of high quality, safe care in this population.
How much does a patient pay for a prescription in 2020?
Their share went from 14.3% in 2019 to 14.9% in 2020. Patients paid an average of $12.36 for a 30-day supply of prescription medication in 2020, an increase of 85¢ vs. 2019.
How much did opioid use fall in 2020?
Opioid utilization fell by 10.3% in 2020, following a 15.2% decline in 2019.
When will cancer drugs be approved?
new cancer drugs approved in 2019 and 2020. Many are firsts for their indication with unique and novel mechanisms of action and treat rare cancers with relatively small patient populations.
What is the purpose of injectable drugs?
These are drugs used to treat rheumatoid arthritis, psoriasis and other autoimmune conditions. Specialty injectable medications account for nearly 95% of medication spend for this class.